9
Pelvic Dysfunction
Pelvic pain can result from numerous body systems including:
| Gastrointestinal | Inflammatory Bowel Disease, Irritable Bowel Syndrome |
| Genitourinary | Bladder Pain Syndrome, recurrent UTIs, Overactive Bladder |
| Gynecologic | Endometriosis, Fibroids, Ovarian Cysts, Pelvic Inflammatory Disease |
| Integumentary | Herpes Simplex, Herpes Zoster |
| Musculoskeletal | Chronic low back pain, Fibromyalgia, tendonitis |
| Neurological | Peripheral Neuropathy, Pundendal Neuralgia, Vulvodynia |
| Psychological | Anxiety, Depression, Trauma |
*This is not an exhaustive list of all the body systems of all of the symptoms that could cause pelvic pain.*
Endometriosis
Endometriosis is where tissue similar to the uterine lining grows outside the uterus, often affecting pelvic organs like the ovaries and fallopian tubes. This can lead to severe pelvic pain, especially during menstruation, significantly impacting daily life.
The condition typically begins with a person’s first menstrual cycle and can last until menopause, often accompanied by inflammation and scar tissue formation. Symptoms may include pain during intimacy, urination, or bowel movements, along with chronic pelvic pain, heavy menstrual bleeding, and gastrointestinal issues such as bloating.
Endometriosis can also complicate conception, and many individuals experience fatigue, depression, and anxiety due to the ongoing physical pain and its effects on reproductive health. Understanding endometriosis is crucial for those affected, highlighting the need for compassionate care and effective treatment options.
Polycystic Ovary Syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that primarily affects menstrual cycles, leading to irregular or prolonged periods. Many individuals with PCOS also produce excessive androgens, resulting in symptoms such as hirsutism, acne, and weight gain. The condition is marked by multiple small fluid-filled cysts on the ovaries, which contain immature eggs that may not ovulate properly, potentially causing infertility.
Symptoms often start in the teenage years and may include polycystic ovaries visible on ultrasound. Managing PCOS typically involves lifestyle changes, like diet and exercise, along with medical treatments to regulate hormonal levels and alleviate specific symptoms.
Pelvic Organ Prolapse
Pelvic organ prolapse occurs when the muscles and tissues that support the pelvic organs, such as the uterus, bladder, and rectum, weaken or become loose. This weakening can be due to damage in the muscles and tissues, causing one or more pelvic organs to drop or bulge into or out of the vagina.
Pelvic organs: vagina, uterus and cervix, bladder, rectum
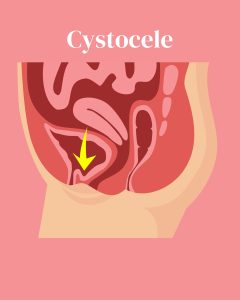
Cystocele (dropped bladder)
This type of pelvic organ prolapse occurs most frequently when the bladder drops into or out of the vagina.
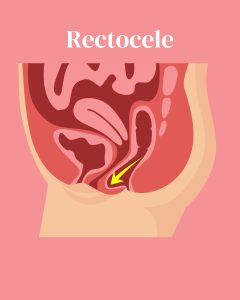
Rectocele
This occurs when the rectum protrudes into or out of the vagina.
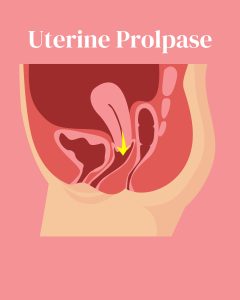
Uterine Prolapse
This condition occurs when the uterus protrudes into or out of the vagina. It may also be related to small bowel prolapse, known as “enterocele,” when part of the small intestine protrudes into the vagina.
Hypertonic vs Hypotonic Pelvic Floor
 The distinction between hypertonic and hypotonic pelvic floors lies primarily in the tone and strength of the pelvic muscles. A hypotonic pelvic floor is marked by a state of weakness and diminished muscle tone, like a once-vibrant balloon that has lost its air. This condition can lead to a variety of issues, including pelvic organ prolapse and urinary incontinence. The compromised strength of these muscles fails to provide adequate support for the bladder, uterus, and rectum, resulting in a cascade of discomfort and dysfunction.
The distinction between hypertonic and hypotonic pelvic floors lies primarily in the tone and strength of the pelvic muscles. A hypotonic pelvic floor is marked by a state of weakness and diminished muscle tone, like a once-vibrant balloon that has lost its air. This condition can lead to a variety of issues, including pelvic organ prolapse and urinary incontinence. The compromised strength of these muscles fails to provide adequate support for the bladder, uterus, and rectum, resulting in a cascade of discomfort and dysfunction.
 In contrast, a hypertonic pelvic floor presents an entirely different picture—one of excessive tightness and involuntary contraction. This condition often stems from heightened tension and stress, manifesting in discomfort, pain during intimacy, and even chronic pelvic pain syndromes. The excessively contracted muscles can create a suffocating environment, hindering normal functioning and restricting blood flow, which can exacerbate the cycle of pain.
In contrast, a hypertonic pelvic floor presents an entirely different picture—one of excessive tightness and involuntary contraction. This condition often stems from heightened tension and stress, manifesting in discomfort, pain during intimacy, and even chronic pelvic pain syndromes. The excessively contracted muscles can create a suffocating environment, hindering normal functioning and restricting blood flow, which can exacerbate the cycle of pain.
Grasping the nuances between these two conditions is essential for pinpointing effective therapeutic interventions and ultimately enhancing pelvic health. By understanding these differences, individuals can embark on a journey toward recovery and well-being.
Hypotonic Pelvic Floor:
Hypotonic pelvic floor issues arise from weakened or overly relaxed pelvic floor muscles. A common problem is stress incontinence, which leads to involuntary urine leakage during activities like laughing or exercising. Urge incontinence is another type, marked by a sudden need to urinate, often resulting in leakage before one can reach the bathroom. Overflow incontinence occurs when the bladder doesn’t empty completely, causing frequent dribbling.
Pelvic Organ Prolapse (POP) is also associated with hypotonic muscles, where pelvic organs like the bladder or uterus descend into the vaginal canal, causing discomfort or a sensation of heaviness. Additionally, these issues can impact sexual function, affecting arousal and orgasm. Recognizing and addressing hypotonic pelvic floor problems is important for improving quality of life.
Hypertonic Pelvic Floor:
Hypertonic pelvic floor disorders include various conditions that can greatly affect quality of life. Common issues are pelvic pain, which may feel constant or sharp, especially during sitting, standing, or exercising. Painful intercourse (dyspareunia) can cause emotional and physical distress, complicating intimacy. Vaginismus involves involuntary pelvic muscle contractions, leading to pain and anxiety during penetration. Vulvodynia is characterized by chronic vulvar pain without clear cause, increasing sensitivity and irritation. Individuals may also face bladder and bowel control issues, such as urgency or incontinence. These disorders highlight the need to address pelvic health comprehensively.
Key Takeaways
- A cystocele is a condition that occurs when the bladder descends into the vaginal canal. Similarly, a rectocele refers to the protrusion of the rectum into the vagina. Uterine prolapse, on the other hand, happens when the uterus shifts and protrudes into the vaginal space. Each of these conditions involves the displacement of pelvic organs and can affect a woman’s health and quality of life.
- A hypertonic bladder is a condition characterized by overly tight bladder muscles, which can lead to issues such as difficulty in urination or increased pressure. In contrast, a hypotonic bladder refers to bladder muscles that lack sufficient strength, resulting in problems like urinary retention or incontinence.
Exercises
- How might a hypertonic pelvic floor be different than a hypotonic pelvic floor during daily living?
Explore
- “Tight & Weak or Loose & Weak: Hypertonic vs. Hypotonic Pelvic Floor Muscles”
- “Occupational Therapy & Pelvic Health: A General Practitioners Guide to Pelvic Floor Dysfunction Throughout the Lifespan”
- “Pelvic Muscle Dysfunction and Continence Improvement” A Primer for Occupational Therapy”
- “Understanding Pelvic Organ Prolapse: Bladder vs. Uterine Prolapse”
References:
Mayo Clinic. (2022, September 8). Polycystic ovary syndrome (PCOS). https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
Office on Women’s Health. (2021, February 22). Pelvic organ prolapse. https://womenshealth.gov/a-z-topics/pelvic-organ-prolapse
Smith, C. (2024, November 9). Hypotonic vs hypertonic pelvic floor: Key differences. Vitality Therapy and Performance. https://vitalitytulsa.com/hypotonic-vs-hypertonic-pelvic-floor-key-differences/
World Health Organization. (2023, March 24). Endometriosis. https://www.who.int/news-room/fact-sheets/detail/endometriosis#:~:text=Overview,period%20and%20last%20until%20menopause.
Media Attributions
- cystocele
- rectocele
- uterine prolapse
- balloon
- hyper stress
