6 Functional Mobility in the Acute Care Setting
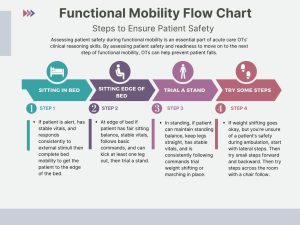
In the hospital, rehabilitation therapy services are often the first healthcare professionals to get patients out of bed. It can be challenging to determine when to progress a patient to each level of mobility. Therapists use their clinical reasoning skills to prioritize patient safety during functional mobility. As you develop your clinical reasoning skills, thinking of progressing mobility in terms of a progressive flow chart may be helpful. Reference the chart below to learn more.
Occupational Engagement at Every Level
Some patients may not be ready for out-of-bed activities. Here are some ideas of various occupations you can do at each level of mobility.
Level 1
Bed Level Activities
- Donning socks in supine
- Supine lower body dressing
- Washing face with a washcloth
- Combing hair
Level 2
Seated Edge of Bed (EOB) Activities
- Donning socks at the edge of the bed
- Upper body dressing
- Brushing teeth
- Training with reachers, sock aids, and shoe horns
- Fine motor coordination
Level 3
Activities Standing EOB
- Lower body dressing
- Training with new assistive devices (walker, cane, etc.)
- Strengthening/ROM exercises to increase independence in ADL tasks
- Functional reaching tasks
- Squat pivot transfers
- To bedside chair or bedside commode
Level 4
Activities that Promote Increased Standing Tolerance and/or Ambulation
- Standing ADLs at the sink
- Toileting in bathroom
- Kitchen tasks
- Full body dressing
BMAT: Interprofessional Approach to High-Quality Patient Care
A tool commonly used to communicate a patient’s mobility level is the BMAT or “Bedside Mobility Assessment Tool for Nurses.” A patient’s BMAT level can be shared in their chart and posted in their room so the care team knows the safest mobility level for patients.
Click here to access the BMAT screening tool.
Functional Mobility Review
Bed Mobility:
Supine to Sit:
Sit-to-Stand Transfer
