5 Cardiovascular Disease Is The Largest Thread to Lives Worldwide
Sabine Zempleni and Eric Hanzel
In December 2020 the WHO published the top 10 leading causes of death worldwide. The data showed major changes during the last 20 years especially in low- and middle-income countries. Have a look at the next infographic or go to the WHO page to read about it.
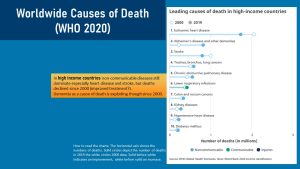
What stands out is that death from CVD—combined death from heart disease and stroke—is the number one cause of death across the world. In low-and middle income countries death from CVD is rapidly on the rise since 2000. In high income countries CVD is still the number 1 cause of death but medical progress and prevention made the disease less deadly over the last twenty years. Death from T2D and hypertension made it into the list for middle income countries as well.
While the reasons for this shift in low- and middle income countries is not well researched, it is generally assumed that the rise in deaths from heart attacks and stroke tends to be the result of the increasing availability of cheap processed foods and sugary beverages. The cheap processed foods replaced the healthy traditional whole foods fare. When the development of CVD meets an inadequate health care system people tend to die from CVD related complications at a much higher rate than people in high-income countries.
The first step of reducing the prevalence of CVD would be awareness. A few recent studies have focused on population awareness of the disease in the US. These studies found that over half of Americans are unaware of symptoms and complications of CVD. On the other hand misinformation in media and social media is rampant. Diets such as Paleo and Keto earn money with the fear of many Americans. Superfoods and supplements are peddled promising to reverse and prevent CVD. What do we really know based on the scientific evidence?
During the last two chapters you already learned that obesity, T2D and hypertension are connected to the development of CVD. In this chapter you will learn how and why CVD develops and how obesity, T2D and hypertension contribute to an acceleration of this chronic disease.
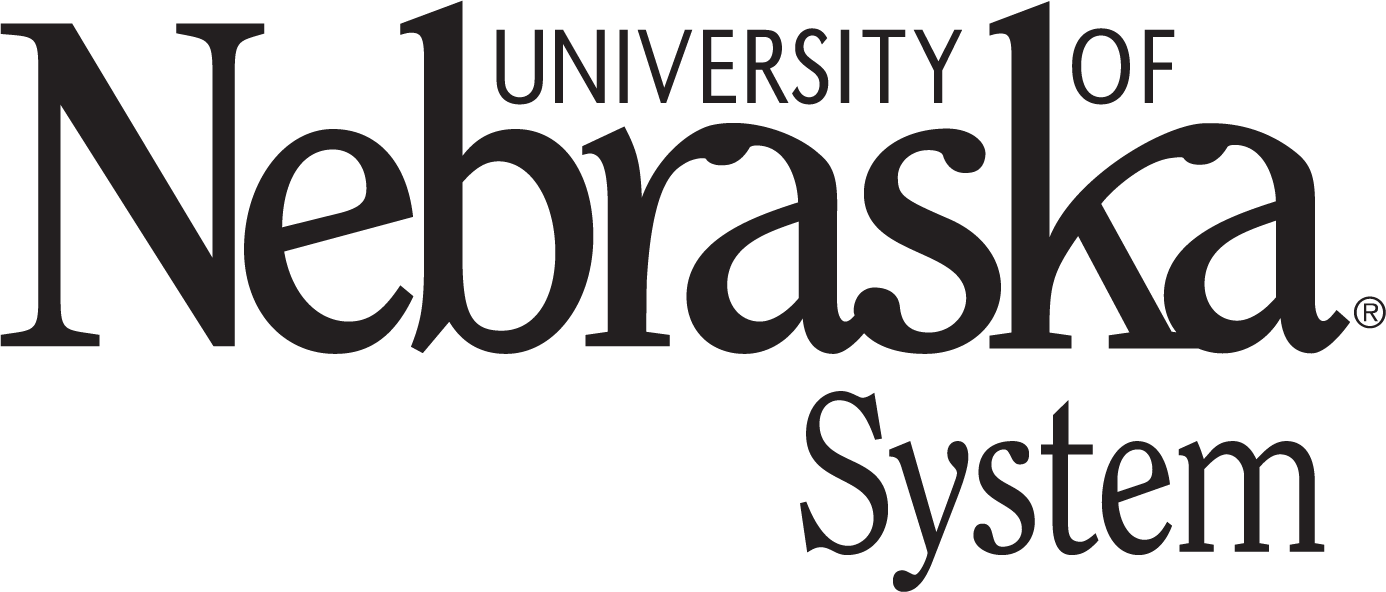
Before you start working on the chapter make sure you review the following infographic refreshing your knowledge about food cholesterol and cholesterol metabolism.
You Will Learn:
- Cardiovascular disease (CVD) is a complex lifestyle disease developing over decades:
- Every person will develop some atherosclerosis over a lifetime.
- A genetic predisposition speeds up the development of atherosclerosis.
- An unhealthy lifestyle speeds CVD up with or without a genetic predisposition.
- CVD, obesity, hypertension and type 2 diabetes are interconnected.
- The beginning of the end? Atherosclerosis is a long-term inflammatory process resulting in CVD and potentially death:
- Atherosclerosis starts as a fatty streak in a vulnerable spot in the arteries and turns into an inflammatory disease.
- Fatty streaks progress into fibrous lesions.
- Plaques become unstable and rupture causing stroke, myocardial infarction, or peripheral vascular disease.
- Lifestyle modifications can prevent progression of atherosclerosis.
- Dietary interventions include a plant heavy diet, replacement of saturated fat with MUFA and PUFA, increased intake of n-3 fatty acids and reduction of added sugar intake.
- Exercise intervention goes hand in hand with dietary intervention and includes 30 – 60 minutes of combined strength training and moderate intensity aerobic exercise on at least 4 days of the week. In addition adopt a physically active lifestyle.
- A weight loss of 5 – 10 % will improve metabolic health.
- Research on how to reverse advanced atherosclerotic lesions is ongoing.
Cardiovascular Disease (CVD) Is a Complex Lifestyle Disease Developing Over Decades
Every person, no matter how healthy, will develop some degree of atherosclerosis during life. A majority of Americans will end up experiencing complications from CVD such as heart attack or stroke by the time they are 80 years old.
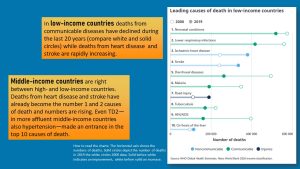
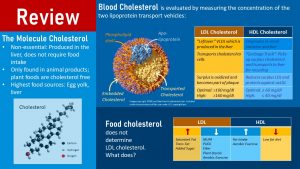
Some Americans will develop symptoms of CVD in high age while others develop CVD in early middle age, sometimes as early as 20 years old (Figure left). The question is why we see those huge differences between individuals.
You already learned about three risk factors accelerating atherosclerosis: Obesity, T2D and hypertension. Those three conditions contribute to epithelial damage and inflammatory processes in the arteries and accelerate the development of CVD. There are many other factors though.
A Genetic Predisposition Speeds Up the Development of Atherosclerosis
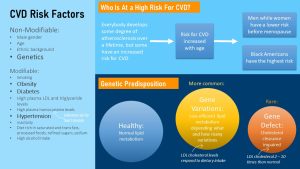
Heart attack in the 30s and 40s especially in male members is running in some families. These families inherit a rare, major gene defect from one generation to the next. This gene defect often effects the interaction between apolipoprotein B and the lipoprotein lipase preventing the efficient uptake of cholesterol by the cell. Familial hypercholesterolemia causes a large increase in lipoproteins especially LDL, an early rapid development of atheriosclerosis, and a high risk for premature heart attack. Lifestyle modifications are not sufficient to lower LDL cholesterol or triglycerides into the normal range. Patients with this gene defect need medical nutrition counselling and drug treatment.
Familial hypercholesterolemia is rare. Much more common are gene variants that don’t automatically lead to skyhigh LDL concentrations. These gene variants impair lipid metabolism to various degrees. This depends on how many gene variants a person has and how severely each variant impacts lipid metabolism. Lately scientists work on developing genetic risk scores that predict who is a high risk for CVD and who is not.
Here is the good news: Ultimately, how much those gene variants impact blood lipids will depend on diet and overall lifestyle. Gene variants combined with an unhealthy lifestyle will generate more readily the atherogenic blood lipid profile—high triglycerides, high LDL and low HDL—that speeds up atherosclerosis and increases the risk for heart attack and stroke. Over 50 % of the fasting and postprandial lipoprotein concentrations are determined by genetic variations. The good news is that for those people the LDL cholesterol levels respond well to diet and exercise.
Lastly there are people that have a very efficient lipid metabolism. Eating saturated fat and cholesterol does not affect blood lipids too much. This lucky group of people develops atherosclerosis late in life.
An Unhealthy Lifestyle Speeds Things Up With Or Without a Genetic Predisposition
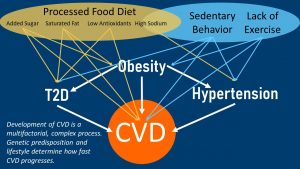
While the genetic variants determines our non-modifiable risk for developing CVD, the onset and progression of atherosclerosis is heavily influenced by our lifestyle. The image above highlights how complex CVD is. Dietary factors and physical activity are intertwined and together lead to CVD. You may notice that most dietary risk factors, and a lack of exercise and physical activity contribute to other chronic diseases as well which in turn contribute to CVD. And, we haven’t even talked about cigarette smoking and chronic stress.
This image should make it clear that it is difficult to contribute the onset of CVD to one factor such as saturated fat. Usually disease progression will be an accumulation of many lifestyle factors.
So now you may ask, “How do I even know I have CVD”….. Well, since nobody can just look into your blood vessels CVD is only detected when complications start. Most people are dignosed when they experience symptoms such as chest pain, chest tightness, shortness of breath, or pain, numbness and coldness in legs. At this point CVD has already progressed far. Before that, all we can do is making active decisions to not engage in a lifestyle increasing the risk for CVD.
What We Do and Don’t Know About CVD:
- Are the effects of CVD reversible? Can certain foods or supplements reverses CVD? A few recent studies have brought to light the potential of drugs and lifestyle changes that might reverse advanced CVD. At this point the focus is more on slowing down or stopping the disease progression though.
- You might have followed the discussion in the media. Does saturated fat intake contribute to CVD deaths or not. A few observational studies found no association between saturated fat intake, high blood cholesterol and death from CVD. The scientists—especially proponents of Paleo and keto diets—proposed that saturated fat is not the issue. Those studies often focus solely on saturated fat and miss a lot of other factors contributing to CVD. Saturated fat can be consumed as part of a healthy diet or part of an unhealthy processed food diet. People can metabolize saturated fat in different ways. Recent research generated evidence that explains the role of saturated fat and the many other contributing factors in a nuanced way. In general the focus of newer research looks more into eating patterns than individual nutrients.
The Beginning Of the End? Atherosclerosis Is a Long-term Inflammatory Process Resulting in CVD And Potentially Death
Imagine sitting on your couch at home. You’re eating your second Big Mac Meal of day and watching Friends for the third time through. You also did the same thing yesterday, the day before, and a few time last week because its been “one of those months”. That doesn’t even account for the snacks you ate while studying for OChem. In the meanwhile the high saturated fat and added sugar intake and your lack of physical activity are getting to work on your arteries. So let me take you on a cardiac adventure, where we will dive into the interworking of our anatomy and explore the cascade of events that unfold in someone developing CVD.
Atherosclerosis Starts As a Fatty Streak in Vulnerable Spots of the Circulatory System And Turns Into An Inflammatory Disease Over Time
Atherosclerosis does not just start anywhere in the circulatory system, but in specific vulnerable spots. Usually the shear forces of the blood flowing through arteries massage the endothelial cells and stimulates healthy cell metabolism. This process helps maintain a healthy semi-permeable barrier function. In some vulnerable spots though, for example when large arteries branche, the shear forces brush less optimally against the endothelial cells.
Atherosclerosis starts in those vulnerable spots.
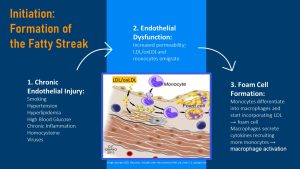
Endothelial Dysfunction: The first step of atherosclerosis is an injury to the artery endothelium (see the review slide above). Injuries always activate the innate immune system which starts the repair process. Repair increases inflammation in the injured area. The injuries can be caused by viruses and auto-immune processes, circulating chemicals from smoking, low grade chronic inflammation due to obesity, hypertension, or high blood glucose concentrations. Over time the blood vessel endothelium becomes weaker and more permeable. The more injuries the faster the endothelium is weakend in those vulnerable spots.
This weakening is called endothelial dysfunction. Since the injured endothelium is weak and more permeable LDL, especially the oxidized form (oxLDL) can now infiltrate the intima. The higher the blood LDL concentrations and the more oxLDL circulates the more is taken up.
Since the endothelium is injured and a substance that shouldn’t be there, oxLDL, is now in the intima endothelial cells call in monocytes to clean up the oxLDL mess.
Macrophage Activation and Foam Cell Formation: The arriving monocytes attach to the endothelium and migrate also into the intima. The weaker the endothelium the better can the monocytes attach. Next, monocytes differentiate into macrophages—macrophage activation—and the macrophages start gobbling up the LDL. These cholesterol filled macrophages are called foam cells.
Macrophages are not just removing waste products, but they also send out cytokine signal to communicate the inflammatory process to other cells and tissues. The secretion of cytokines recruits more monocytes and other immune cells. Since inflammation is damaging the endothelium further the atherosclerotic process goes now into an inflammatory spiral.
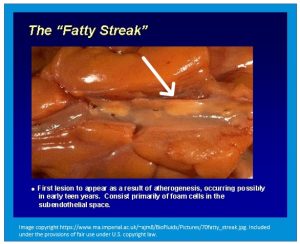
If you would cut open the artery at this point you would see a yellowish white fatty streak in the artery wall (picture to the right.)
At this early stage, especially if HDL concentrations are high and LDL concentrations are low, HDL will lock on to the epithelium and absorb the surplus cholesterol almost like a little vacuums.
Fatty Streaks Progress Into Fibrous Lesions
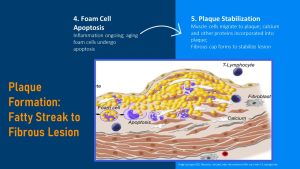
If the lifestyle doesn’t improve atherosclerosis progresses. As the cholesterol filled foam cells keep building up and age. At one point in their life the foam cell will undergo apoptosis releasing cholesterol and cell fragments into the intima.
Plaque Stabilization: The cholesterol and macrophage fragments accumulate as plaque in the blood vessel intima. The plaque is soft and unstable and this elicits a physiological response to stabilize. Smooth muscle cells are recruited and together with other proteins such as collagen and calcium from the blood the core is becoming fibrous and stabilized, but also harder. A fibrous cap forms on top of the fibrous lesion.
Keep in mind that the material from the fibrous lesion is not supposed to be in the blood vessel intima. Therefore the immune system keeps recruiting immune cells to the lesion and the inflammatory process foments the expanding of the fibrous lesion and narrowing of the artery.
Endothelial stiffness: As plaque continues to build up and is getting harder arteries become not only narrower, but due to the fibrous plaque also stiffer. One of the first measurable signs of CVD is endothelial stiffness. Stiffer and narrower arteries will require a higher blood pressure to pump blood through. This contributes to hypertension which causes more microtears to blood vessel endothelium starting more atherosclerotic spots.
When arteries narrow noticeable symptoms develop. The increased stress on the heart muscle and reduced blood flow might lead to fatigue, breathlessness, rapid heart rates, and chest pain. Narrowed arteries in the legs can cause leg pain.
Now you should also understand how hypertension and T2D aggravate CVD. Hypertension increases injury to the artery endothelium due to the constant increased pressure against the artery walls. Think about a massage with high pressure that does not let up. High, fluctuating blood glucose and free fatty acid concentrations in pre-diabetes and diabetes are cell toxic and damage the endothelial cells increasing permeability (glucolipotoxicity.)
Plaques Become Unstable And Rupture Causing Stroke, Myocardial Infarction, Peripheral Vascular Disease And Potentially Death
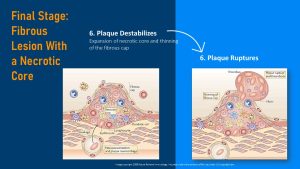
The necrotic core: As the atherosclerotic lesion growths the foam cell breakdown continues and the material under the fibrous cap grows into a softer and increasingly larger unstable lesion. This is called the necrotic core.
As the necrotic core grows the fibrous cap is stretching and damages to the fibrous cap make the atherosclerotic plaque prone to rupture. Left unchecked, the Big Mac Attacker’s plaque infested artery walls will become unstable, rupture and a blood clot will form around the ruptured plaque.
The ruptured plaque can now completely block the artery or pieces of the blood clot might break off and start traveling. Unfortunately we need blood flow to live. When arteries are blocked blood flow to the surrounding tissue stops and tissue dies. Consequently, complications occur and might result in death if not treated quickly.
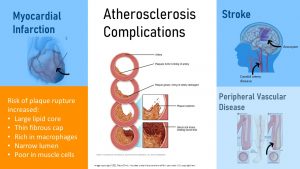
CVD complications are:
- Stroke: Two scenarios are possible. A blocked artery reduces or stops the blood flow to the brain or to parts of the brain. The second scenario is an unstable artery in the brain rupturing and bleeding into the surrounding brain tissue (aneurysm.) Both variations will cause damage to brain tissue. Once the brain stops receiving the necessary nutrients and oxygen from the blood, brain cells will begin to die. If treated immediately, extensive brain damage might be prevented. Symptoms of a stroke include, trouble speaking or comprehending, paralysis or numbness in face, arms, or legs, difficulties with opening and closing eyes, headaches, and trouble walking. Depending how large the damaged brain area is and what area of the brain is affected the stroke might be fatal.
- Myocardial Infarction: More commonly known as a heart attack, this occurs when blood flow to a part of the heart muscle is blocked. Lack of oxygen leads to muscle cell death and the heart stops working properly. Immediate medical attention should be sought in order to prevent extensive cardiovascular damage or death. Symptoms of a myocardial infarction include pressure, tightness or pain in the chest, arms, neck, or jaw, nausea or indigestion, shortness of breath, fatigue, lightheadedness, and cold sweats. Heartattacks in women tend to be more deadly because women often do not experience the typical symptoms such as chest or arm pain. Often their symptom seem unrelated such as fatigue, nausea, indigestion, or feeling of pressure.
- Peripheral Vascular Disease: This disease is caused by reduced blood flow to the body’s limbs – mostly the legs. While not necessarily fatal, it indicates that plaque build-ups are starting to reduce blood flow. Symptoms of peripheral vascular disease include pain or cramping in legs during exercise, blue discoloration in legs, and numbness.
As the blood flow stops, so does the end of our cardiovascular adventure…. Are you starting to piece together the big picture? While the Big Mac example may be a little dramatic, it represents the cascading effects of cardiovascular destruction that unfolds IF left unchecked.
A New Beginning: Modifying your lifestyle to prevent and reverse the affects of CVD
A Lifelong Healthy Lifestyle Will Slow Down Atherosclerosis

Notice how I left you in the last section with “IF left unchecked” because who doesn’t love a cliffhanger?
Even the healthiest person will develop some degree of atherosclerosis over the lifetime. The key is to slow atherosclerosis down as much as possible with an overall healthy lifestyle.
There are several non-modifiable risk factors. You already learned about genetic predisposition and age as non-modifiable risk factors. Here are two more:
Gender: Women have a lower risk to develop atherosclerosis and CVD than men up until they go through menopause. After menopause their risk is similar to men. The hormon estrogen has a protective effect. A few years before menopause estrogen production declines along with the protective effect.
Racial Differences: Black men and women have the highest rates of heart failure, peripheral artery disease and stroke. Even if the rates of coronary artery disease are lower in Black Americans than Whites mortality from heart attack is higher. Causes discussed are a higher rate of T2D, hypertension and obesity especially in Black women. Socio-demographic factors such as less access to preventative health care play a role. Pathophysiology in Black Americans is little researched and therefore recommended lifestyle interventions and CVD treatment might not be as efficient in Black Americans.
The good news is that studies show that lifelong healthy lifestyle—meeting 3 of the 4 criteria below— compared to an unhealthy one is cutting the risk for the dreaded coronary artery disease almost in half. This applies for both, people with or without genetic predisposition.
This healthy lifestyle consists of:
- Changes to your diet: Decreasing the intake of saturated fat and added sugar—all those quick fast food meals and convenient snacks—can decrease the risk of acquiring CVD. Processed foods don’t need to be eliminated completely but daily eating should be centered around plant-heavy, fresh foods.
- Changes to your physical activity and exercise: Increasing the amount of daily activity and decreasing the amount of sedentary time can decrease the risk of acquiring CVD. Vigorous aerobic exercise is a great prevention tool.
- Maintain a healthy weight: A plant heavy diet combined with loads of physical activity should keep the weight healthy as well. Keep in mind that a healthy weight is not what you see on Instagram.
- Changes to other health behaviors: Decreasing exposure to smoking, sufficient sleep, reducing stress and moderate consumption of alcohol will decrease the risk of acquiring CVD.
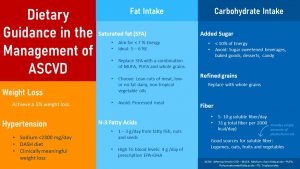
LDL And HDL Cholesterol Is Kept In Balance By Eating a Plant Heavy Diet And Reducing Processed Foods
The question is now how eating needs to change if somebody is diagnosed with atherosclerosis or CVD. Thinking back to the development of artherosclerosis there are two moving factors: Inflammation and the amount of LDL cholesterol circulating. Dietary intervention addresses those two factors and has four major goals:
- Reducing LDL cholesterol
- Increasing HDL cholesterol
- Reducing chronic systemic inflammation
- Reducing sodium intake
While cholesterol and saturated fats have been portrayed as the villains in this dramatic telling, both nutrients are not inherently unhealthy. Both have metabolic functions and don’t need to be completely eliminated.
Cholesterol found in circulating lipoproteins stems either from animal foods (plant foods are cholesterol free) or is produced endogenously in the liver. Dietary and endogenous cholesterol is packed in the liver along with triglycerides and other fat-soluble nutrients into lipoproteins.
The lipoproteins then circulate the blood stream like a Dim Sum cart. Cells take what they need shrinking the lipoproteins in the process. What is left after all energy rich lipids are removed from the cart is circulating cholesterol, the LDL. Cells keep taking cholesterol to build cell membranes or to synthesize steroid hormones. This way cholesterol helps maintain the structure and function of cell membranes and aids regulation of the metabolism.
Surplus LDL cholesterol keeps circulating and after a while LDL is oxidized. As you learned above the oxLDL passes through the artery endothelium, is gobbled up by the macrophages and contributes to the plaque build-up. The higher the circulating LDL and lower the HDL concentrations the faster artery plaques grow.
HDL functions as mini-garbage trucks, circulating the blood stream and remove surplus LDL before it can be oxidized. Newer research hints that HDL might also help vacuum cholesterol from existing plaque.
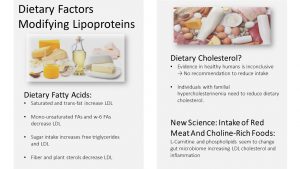
What dietary factors are driving the LDL cholesterol up? It’s not the dietary cholesterol as many assume.
As stated previously, cholesterol is a non-essential nutrient and produced in the liver. The human liver is producing all the cholesterol we need to function normally. The cholesterol we consume from meat and other animal products, referred to as dietary cholesterol, is actually all excess. For healthy individuals, diving into a couple big macs or eating a breakfast egg will not speed up atherosclerosis. The metabolism will just reduce how much cholesterol is produced by the liver. Therefore, healthy individuals do not need to watch their cholesterol intake. Those with familial hypercholesterinemia (gene defect) and a history of CVD however are recommended to reduce foods rich in cholesterol.
Saturated Fats on the other hand are more bad than good. Like all fats, saturated fat will still provide energy, increase fat-soluble vitamin absorption, as well as aid in protection of organs and tissues in form of essential body fat.
The bad part about saturated fats is that they increase the amount of LDL cholesterol. Keep in mind though that all foods contain some amount of saturated fat, some more, some less. When we eat a lot of foods that contain saturated fatty acids as their predominant fat we see the LDL rising. This affects especially people with the gene variants or gene defects.
In the past the recommendation reducing saturated fat was interpreted as eat low-fat foods only. This resulted in processed, fat-free or low-fat food products containing a lot of starches and sugar to mimic the creamy, silky texture of fatty foods.
Today we know better. Reducing saturated fat without replacing it with healthier fat has an undesired side effect. A low fat diet will reduce LDL as desired. But, a low fat diet will also reduce the beneficial HDL. This lead to a different recommendation: Replace foods high in saturated fat with foods containing predominantly mono- and polyunsaturated fats. Since we don’t eat saturated and unsaturated fat but foods, how does this look in practice? Foods high in saturated fat—red meat, cheese, eggs—should be eaten in moderation and the excess should be replaced with foods higher in poly- and mono-unsaturated fats—fish, plants fats, vegetable oils. This strategy will help keep LDL in check and allows HDL to remove excess LDL and fatty deposits in the arteries.
Added Sugar: High sugar intake is another contributor to the development of CVD that we haven’t touched base on much. While carbohydrates are necessary to provide our bodies with energy, too much of the wrong kind, sugars and starches, will cause an increase in free triglycerides that subsequently increases the amount of LDL.
Low-fat processed foods taste terrible. So food scientists set out to improve the eating experience of low-fat products by adding starches, saccharose and other nutritive sweeteners. This improves the flavor profile—who doesn’t like sweet and salty—and nudges the dry, chewy texture to silky and smooth. These sweeteners can be found in sweet foods and foods we wouldn’t expect them such as a can of beans. Since Americans eat a lot of processed and convenience food they eat a lot of those unhealthy carbohydrates.
How about low-carb diets or the keto diet? You might have noticed that I talked about the wrong kind of carbohydrates. There is ample amount of evidence that supports eating the right kinds of carbohydrates—whole grains, legumes, starchy vegetables all rich in complex carbohydrates and fiber—to reduce LDL and in consequence prevent CVD.
Soluble Fiber and Plant Sterols: Whole grains, legumes, fruits and vegetables provide ample amounts of fiber and one kind in particular. Soluble fiber reduces the absorption of food cholesterol and bile. When HDL bring cholesterol back to the liver some is recycled and send back out into the circulation. The liver also uses this cholesterol to produce bile. Bile is stored in the gall bladder until it is secreted into the duodenum during fat digestion to emulsify the fat.
Usually, bile is re-absorbed in the lower parts of the small intestine. In the presence of ample amounts of soluble fiber some cholesterol from food and bile attaches to the fiber which makes it unavailable for absorption.
Plant sterols have a similar chemical structure than cholesterol and compete with cholesterol for absorption. If plenty of plant sterols are present some cholesterol is left without a ride into the brush border cell. In consequence cholesterol is excreted in the feces lowering the amount of endogenous and dietary cholesterol circulating in the lipoproteins. By the way, preventing re-absorption of bile is the only way to excrete surplus cholesterol.
Omega 3 Fatty Acids Lower Triglycerides, Reduce Chronic Systemic Inflammation And Improve Endothelial Function
Another promising research area is the connection between n-3 fatty acids and the development of CVD. Studies show that especially n-3 fatty acids from marine, fatty fish can slow down or maybe reverse the development of CVD. Increased intake of n-3 fatty acids lower triglyceride concentrations and positively effect other risk factors such as inflammatory processes, thrombosis and endothelial function.
Fish oil supplements for individuals with CVD are discussed as well. Prescription supplements are sometimes prescribed in high-risk patients with high blood triglycerides. The doses of those prescription supplements are higher than what you find in a drug store supplement. For everybody else over-the-counter supplements are not worth the money because studies do not show an improvement of CVD. Interestingly, studies show a risk reduction if people eat fish. N-3 fatty acids from plant sources such as nuts show some improvement but not as much as the ones from sea food. At this point this discrepancy is puzzling. So, rather eat fish than popping an over-the-counter supplement.
Sufficient Amounts of Antioxidants From Fruits And Vegetables Reduce Chronic Systemic Inflammation
Plant foods do not only deliver healthy fats and ample amounts of fiber, but they are the main source for antioxidants and phytochemicals. Newer evidence shows that these plant-derived antioxidants are able to reduce chronic systemic inflammation.
Keep in mind that this doesn’t mean to take an antioxidant supplement or eating “super” fruits helps more. Americans tend to eat a processed food heavy diet and very little fruits and vegetables. This leaves them short in antioxidants and phytochemicals. The strategy is to up the plant food intake to have a sufficient amount of antioxidants and phytochemicals in the diet.
Three dietary patterns are are fitting those dietary strategies and are therefore recommended for the prevention and treatment of CVD:
- Healthy American eating pattern such as DASH diet
- Mediterranean eating pattern
- Vegetarian eating pattern
The following figure summarizes the recommendations for individuals with CVD:
Physical Activity and Exercise Improve Health
While eating healthy is a great strategy to reduce the risk for CVD other lifestyle factors should be addressed as well such as having an active lifestyle, reducing stress and getting enough sleep. While exercising will not necessarily fix obesity on it’s own, the impact of aerobic exercise on heart health is extensive.
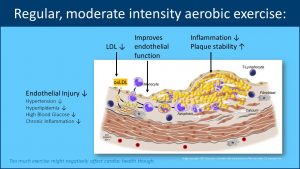
Studies have shown that that currently, on average, Americans spend about 7 hours a day being sedentary. Additional studies that have looked at how sedentary time affects risk of developing CVD has shown associations between increased risks of CVD at 6-8 hours of sedentary time and an even higher risk once passed the 6-8 hour threshold. High amounts of sedentary time even seem to increase CVD risk if people exercise regularly.
Based on this evidence moderate intensity aerobic exercise for at least 150 minutes a week or 30 minutes for 5 days a week has been a staple recommendation to improving overall cardiovascular health. Benefits include:
- Decreased endothelial injury resulting from decreased levels of hypertension, hyperlipidemia, hyperglycemia, and inflammation.
- Increases in endothelial function resulting from decreased levels of LDL and macrophage differentiation.
- Decrease in plaque formation caused by decreases in smooth muscle cell proliferation
The best part about aerobic exercise is that it can be done in a variety of ways including jogging, bicycling, weight lifting , or your favorite sport/activity. While aerobic activities such as these have a good amount of solid evidence to their name when it comes to cardiovascular health.
Anaerobic exercise such as weight lifting has shown mixed results when it comes to CVD. Strength training should still be included in an exercise regime though because the increase in muscle mass will increase the RMR and therefore make weight maintenance easier.
High-Intensity intermitted exercise has been shown to improve cardiovascular health similar to aerobic and in some cases actually showed better overall improvements. However, the disadvantages of high-intensity training is its effects on increasing blood pressure that can exacerbate pre-existing CVD complications. Its best to conduct this type of training under strict supervision. Also, HITT exercise is advertized as a time saver. This should not mean that one can spend the rest of the day at the desk or on the couch.
Is there no going back?
While it is best to prevent CVD in childhood and young adulthood learning healthy lifestyle habits, many middle aged adults wonder if the damage can be reversed once they are dianosed with hypertension, pre-diabetes or CVD.
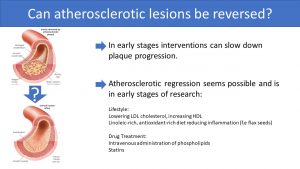
Studies show that lifestyle intervention and drug therapy can slow down the progression of atherosclerosis.
The question is if the damage can be reversed as well. The research is in an early stage though. Promising strategies intentionally increasing linoleic acid (for example from flax seeds) and antioxidants in the diet.
Recent studies have also shown that the effects of atherosclerosis might be reversed with proper lifestyle changes and drug adherence. Adopting the health behaviors mentioned above along with intravenous administration of phospholipids seem promising to improve atherosclerotic damage. Statin drugs also show some promise. With ongoing research developing in both the reversal process of CVD and establishing better awareness, we will hopefully start to see increases in overall health and well-being in our populations.
Interested In More Information?
- Sapp PA et al. Nutrition And Atherosclerotic Cardiovascular Disease. In: Marriott BP, Birt DF, Stallings VA, Yates AA eds. Present Knowledge in Nutrition: Volume 2: Clinical And Applied Topics in Nutrition. London, United Kingdom: Elsevier; 2020:361-377.
- Byrd-Bredbenner C, Moe G, Berning J, Kelley D. Wardlaw’s Perspectives in Nutrition. New York, NY: McGraw-Hill Education; 2019: 193-227
- Hudson L, Yaqoob P. Fat Metabolism. In: Geissler C, Powers H eds. Human Nutrition. Oxford, UK: Oxford University Press; 2017:161-183
- American Heart Association: https://www.heart.org/
- CDC: https://www.cdc.gov/heartdisease/index.htm
Editors: Nicole Legler, Gabi Ziegler
NUTR251 Contributors:
- Spring 2020: Eugene Baraka, Rawan AL Jabri, Kennedie Engles, Maria Lantos, Hazel Lesher, Kealy Barnes, Eugene Baraka, Amelia Johnson, Tim Gillespie
- Fall 2020: Collin Mahler, Clare Caraghar
Lipoproteins secreted right after a meal to transport absorbed fats to cells for use or store in the adipose tissue. These include chylomicrons, VLDL, LDL and HDL which are all elevated after a meal.
LDL can be damaged by free radicals. This can happen in the blood stream where oxidative capacity is high due to the present oxygen or after in the blood vessel intima by radical oxygen species.
cell death
Plaque is made from deposits of fatty substances, cholesterol, cellular waste products, calcium, and proteins.
Per definition atherosclerosis is the hardening of the blood vessels and meansured by determining the endothelial stiffness. Both endothelial dysfunction and stiffness are used as biomarkers for the risk of CVD. Endothelial or arterial stiffness is measured in clinical settings using ultrasund techniques.
Atherosclerosis of the coronary arteries
Resting metabolic rate


Feedback/Errata