17 Human Milk Is More Than Nutrition For Infants
Sabine Zempleni; Eric Hanzel; and Sydney Christensen

Congratulations! After many hours of an exhausting labor, you welcome a new tiny human into the world and embrace them in your arms. You treasure the tranquility and accomplishment of this big moment, but as their solemn slumber is slowly replaced with cries of hunger and distress, you realize your work as a parent is just getting started. Thankfully, all through pregnancy the mother’s body has been preparing for this moment—breastfeeding.
During this chapter you will learn about breastmilk production, nutrient composition, and bioactive compounds in human milk.
You Will Learn:
- Pregnancy hormones prepare the mother throughout pregnancy for lactation
- Estrogen, progesterone and prolactin interact to adapt breast tissue for lactation
- After birth prolactin stimulates milk production and oxytocin releases the milk during nursing
- Ruled by reflexes, the newborn is a natural at breastfeeding
- Rooting reflex turns the head toward the nipple and opens the mouth
- Suck and swallow reflex maintain the nursing motions
- Human milk adapts to the need of the infant
- Milk volume, stimulated by the frequency and duration of nursing, increases rapidly during the first month. Then volume increases slow down
- Small but mighty: Colostrum’s function is immunological and developmental, and not so much nutritional
- Colostrum is followed by transitional milk after 5 days, followed by mature milk after 14 days
- Milk composition changes during one feeding and during the day
- Human milk does not just deliver nutrients for growth
- Human milk lipids provide nutrition and bioactive compounds
- Human milk is low in protein and high in carbohydrates compared to animal milk
- Bioactive compounds from human milk set up digestion and immune system
- Immunoglobulins an antimicrobials
- Human made oligosaccharides (HMOs)
- When Breastfeeding Is Not Perfect
- Vegan mothers and vitamin B12 deficiency
- Vitamin D supplementation
- Vitamin K supplementation after birth
- Infections diseases such as HIV and hepatitis B
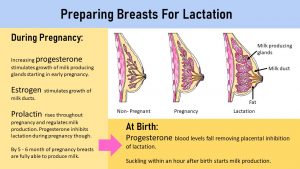
Pregnancy Hormones Prepare the Mother Throughout Pregnancy For Lactation
During Pregnancy
A pregnant woman’s body is not just growing the placenta, uterus, and feeding the fetus. Starting in early pregnancy, the woman’s body is getting ready for breastfeeding. Energy stores are created in the form of adipose tissue and the breast anatomy is altered. These changes are driven by the placenta hormones estradiol and progesterone.
- Estradiol stimulates the growth of milk ducts in the breasts.
- Progesterone stimulates the growth of milk producing glands starting in the first trimester. As levels of progesterone increase throughout the pregnancy so does the development of the glands.
- The third hormone involved in preparing for breastfeeding is prolactin. Prolactin is not produced by the placenta but estrogen and progesterone stimulate the production in the pituitary gland. Prolactin stimulates the production of milk. Levels of prolactin increase throughout pregnancy and are highest after birth, but the pregnant woman is not lactating. Why? During the pregnancy high progesterone blood concentrations are putting the break on prolactin. Before birth, progesterone levels fall and prolactin starts stimulating milk production.
After Birth
The flood gates are now open and the breastfeeding adventures can begin. The actual mechanism of milk production has two parts regulated by two hormones.
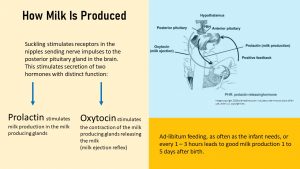
While prolactin secretion was stimulated by the pregnancy hormones, this stimulus is gone after birth. Prolactin production is now stimulated and maintained by the infant (or the pump) suckling on the breast.
When the infant suckles at the breast neuronal impulses are sent to the brain. In response two hormones with two distinct functions are released into the bloodstream.
Prolactin is produced by the anterior pituitary gland and stimulates the milk production in the milk glands. The produced milk is stored in the glands and milk ducts Prolactin blood levels are highest 30 minutes after breast feeding begins. This means that pituitary gland and breast prepare for the next feeding while the infant nurses.
Prolactin has a secondary function. It suppresses the production of GnRH, LH and FSH and therefore suppresses the menstrual cycle. Women need to keep in mind though that this is not a perfect birth control. Especially when breast feeding is supplemented with formula or solids the effect is not sufficient to prevent another pregnancy.
Keep in mind prolactin only stimulates milk production. In order to release the milk the release of a second hormone, oxytocin, is necessary.
You might be familiar with oxytocin which is often called the happiness hormone. Released during hugging it drives us humans to snuggle up with other humans and pets. The release during intensive exercise leads to the famous runner’s high.
Oxytocin is produced by the posterior pituitary gland when the baby latches on and triggers the milk release. This is called the milk-letdown reflex or milk ejection reflex. The alveoli of the milk glands are surrounded by muscles and these muscles contract when stimulated by oxytocin. The milk is literally expressed. Once breastfeeding is fully established oxytocin is already released when the mother expects breastfeeding which leads to leakage. This includes hearing the baby cry, smelling the baby, or even knowing that the next breastfeeding is due any moment.
After delivery oxytocin has also the function to contract the uterus back to a smaller size. This reduces bleeding after birth. Another function is psychological. Oxytocin calms the mother and promotes bonding between the baby and mother.
Oxytocin is also the hormone that can make breastfeeding difficult. If the mother is tense and stressed and unsure about her abilities to breastfeed, oxytocin production is suppressed. Milk is then produced, but not released. This leads to painfully full breasts and a lot of frustration. It is important that the family provides a relaxing, supportive environment for the new mother so she can learn to relax into breastfeeding.
Ruled By Reflexes the Newborn is a Natural At Breastfeeding
After birth newborns go through major adjustments. Their dark and muffled environment in the uterus is traded for the bright and noisy world. The constant warmth of the watery environment in the uterus is replaced by cooler and fluctuating temperatures. The constant flow of nutrients is replaced by feelings of hunger. How does the newborn learn to feed?
With the right guidance and timing breastfeeding can start off well or set everybody up for frustration.
The newborn is in principle a natural at breastfeeding. Finding the breast, latching on (with a little help) and suckling is all guided by reflexes.
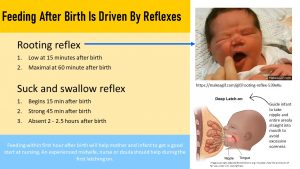
Two reflexes are coordinating the feeding process of the newborn.
Rooting reflex: When the nipple of the breast touches the infant’s face the infant will turn the open mouth towards the touch and search for the nipple.
Suck and swallow reflex: This reflex is developed after 32 weeks of gestation and the fetus will suck on fingers when they get into the mouth in the uterus. This is also how the feeding version works. When the nipple touches the inside of the lips and mouth the infant starts a coordinated sucking and swallowing motion.
Here is some knowledge people in past times when breastfeeding was part of family life knew but is often forgotten today.
The first 15 minutes or so after birth the newborn is exhausted and after the first cry tends to rest. Then things start to happen:
- The rooting reflex is low during those first 15 minutes after birth but then gets stronger reaching a maximum at 60 minutes. After that the reflex declines and the infant gets sleepy.
- The suck and swallow reflex follows a similar pattern. It begins after 15 minutes, is strong at 45 minutes and is absent around 2 hours after birth.
This makes it important that the first breastfeeding takes place in the delivery room. Breastfeeding will not only help the newborn’s GI system to get a boost, but will lead to better uterus contractions and gets mother and baby into a feeding pattern.
It is important though that an experienced delivery nurse or midwife instructs the new mother how to properly latch the baby on. The baby needs to take the entire nipple and areola (dark tissue surrounding the nipple) straight into the mouth. Otherwise the nipples get damaged by the strong sucking to the point of bleeding. Soreness of nipples and areola are common during the first weeks as the tissue gets stronger. Proper latching on will reduce this side effect.
Still, this soreness is often a reason why some new mothers give up breastfeeding too soon. Education about what to expect and how to treat sore breasts will help the mother to get over those initial hurdles. Ideally the new mother will meet several times with a lactation consultant. Studies show that this will make it much more likely that the mother eases into breastfeeding and breastfeeds for the full recommended 6 months exclusively.
It will also help if the new mother knows what to expect. Ad libitum feeding is frequent during the first weeks and seems to consume the entire day. Below are screen captures of a new mother nursing during the first week of the newborns life and then at two months. Each orange bar is a feeding and the height indicates the duration.

Human Milk Adapts to The Need of The Infant
As you will see during the rest of the chapter, breast milk is the ideal food for the baby during the first 6 months. No technological and scientific improvement of formula will be able to mimic the complexity and adaptability of breastmilk.
During the first two days after birth the mother produces only small amounts of milk. This is often misunderstood and misinterpreted. The woman might be told she does not have “enough milk”. Therefore formula is supplemented or the woman is discouraged entirely from breastfeeding.
This situation is based on a misunderstanding of the purpose of colostrum, milk produced during the first days after birth. Colostrum has mainly a physiological purpose—transitioning the immune, gastrointestinal system, and metabolism to life outside the uterus—and less a nutritive purpose. Digestion is not fully functional during these first days and the newborn’s stomach is tiny.
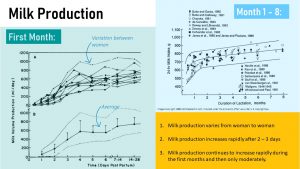
Milk Production Increases Rapidly Until the End of the First Month
After birth women produce anywhere between 10 and 100 ml colostrum per day with an average of 30 ml. How much is 30 ml? About 1 ounce and a cup has 8 ounces. This would only be a sip of milk in a cup.
The turquoise graph above depicts the amount of breastmilk for several mothers (top) and the average (bottom). Three facts become clear from this graph:
- All mothers start with very small amounts of colostrum after birth. This gives the newborn a chance to adapt to oral feeding. The fetus practiced feeding by drinking amniotic fluid in-utero but so far nutrients never reached the GI system.
- During the first month the amount of milk rapidly increases, reaching on average 700 ml (3 cups) at the end of the first month. This is just an average though and that brings me to the third fact.
- How fast milk production increases and how much milk is produced is very individual. This depends partially on the nutritional need of the newborn.
Milk production is stimulated by the neuronal signals sent to the pituitary gland when the infant latches on. The more often the infant latches on the more signals are sent. Practically this means that the infant need to be fed often during the first days to stimulate the milk coming in. It is recommended that the newborn infant is fed during the day every 1 – 3 hours. Most infants will want to feed that often, more sleepy newborns need to be woken up. This frequent feeding will stimulate the milk coming in, as it is often called, and gives mother and infant a chance to practice.
The second cue to increase milk production is the emptying of the breast. The mother should always make sure the infant empties one breast first, then switches to the other. The next feeding will start with the breast that was not emptied.
If the infant has not gained back the birthweight after 10 days—this tends to coincide with the first well-baby check up—the pediatrician needs to investigate. One cause could be a medical problem, the other insufficient milk production. Referral to a lactation consultant can help fix problems and misconceptions. Until breast feeding issues are fixed supplementing formula will be necessary.
One more question to answer. How do we tell how much milk an infant drinks during latching on? To determine the amount of milk an infant drinks the mother would place the infant before she starts feeding on a scale. After the feeding the infant is weight again and the difference is the amount of milk consumed.
After the First Four Weeks Milk Production Increases Only Moderately
Have a look now at the graph in the right upper side of the image above (light blue). This compilation of studies shows the development of milk production during the first 8 months. You see the steep increase during the first months and after that the milk production increases only moderately. You also see large differences in this case between studies.
Around 6 month, for some infants this might happen earlier, the milk production will not be sufficient anymore to fully feed the baby. At this point solids must be introduced to supplement human milk.
It is important that the mother knows that as the infant grows milk amounts need to be adjusted. The infant becomes more hungry, latches on more often and occasionally needs a night feeding even after the infant has already started sleeping through the night. This is normal. At this point mother and infant are an experienced breastfeeding team.
In the US most mothers will have switched to pumping milk after they return to work after week 6.
Small But Mighty: Colostrum’s Function is Immunological and Developmental And Not so Much Nutritional
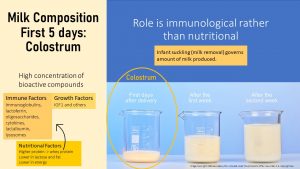
During the first 5 days of breastfeeding, milk composition consists mostly of bioactive compounds such as immune and growth factors along with some nutrients. This stickier and yellow milk is called colostrum.
The main components of colostrum are:
- Immune Factors consisting of immunoglobins, lactoferrins, oligosaccharides, cytokines, lactalbumin, and lysosomes
- Growth Factors consisting of mostly of IGF1 and smaller amounts of other growth hormones
- Nutritional Factors consisting of high protein concentrations (mostly whey protein, see below), lower lactose and lipid concentrations
Overall, colostrum is lower in energy.
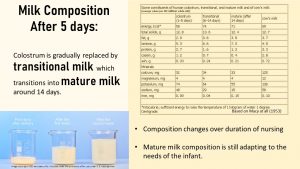
After these first five days have elapsed, colostrum is gradually replaced with transitional milk. Transitional milk has a higher energy content since carbohydrates, lipids and nutritional protein concentrations are increasing. This way the digestive system can slowly learn to digest nutrients until the infant’s digestive system is ready for the mature milk about 14 days later. At this point the milk volume will keep increasing depending on the need of the infant. Composition may not change much but milk-producing glands will continue making adjustments based on the infant’s needs.
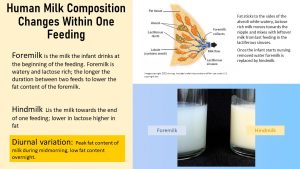
The time and frequency of breastfeeding plays a major role when it comes to milk composition. As milk is made, fat sticks to the sides of the milk-making glands and the watery part of the milk moves down the ducts toward the nipple. The fatty milk stored further up in the milk glands is referred to as hindmilk. Farther down towards the nipple, the newly synthesized milk will mix with any milk left from the last feed referred to as foremilk. The longer the time between feeds, the more diluted the leftover milk becomes. This ‘watery’ milk has a higher lactose content and less fat than the milk stored in the milk-making cells higher up in the breast.
An infant nursing at the breast would first have watery, lactose-rich milk and as the feeding goes on the milk would become more fatty. It is discussed but not clear if this variation of fat and lactose content during one feeding has an effect on hunger and satiety regulation. In addition, milk produced in the morning—fed midmorning—contains more fat while milk synthesized overnight is lower in fat. Today, many infants are fed pumped and pooled milk via a bottle. These infants will still drink milk with different fat concentrations depending when the milk was pumped but the milk will not have the circadian rhythm of composition. So far, the physiological impact of this interesting feature of breast milk is not researched.
Human Milk Does Not Just Deliver Nutrients for Growth
Human Milk Lipids Provide Nutrition and Bioactive Compounds
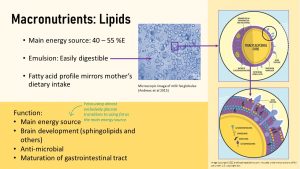
While the fetus used almost exclusively glucose as an energy source, once the infant is born they switch to fat as their main energy source. Around half of the infant’s daily energy intake stems from fat. Breast milk fat is ingenuously packaged into globules that disperse the fat very finely in the watery breast milk. The small globules (see figure above) emulsify the fat effectively, generate a large surface for digestion so human milk fat can be easily digested even with less bile and lipase.
This way of packaging fat should be familiar to you. During human fat digestion bile secreted from the gall bladder emulsifies fat into droplets so lipases can digest it. Without bile fat passes undigested through the digestive system. A similar bilayer structure allows fat to travel in the watery blood as lipoproteins. The human milk globules have an even more unique tri-layer structure.
Milk fat globular membranes (MFGM) contain four key compounds arranged in three layers: Glycerophospholipids, sphingolipids, cholesterol, and glycosphingolipids. Most mammal milk contains MFGM but human milk globules are much smaller than animal globules. In addition, if milk is heated for example during pasteurization the MFGM is damaged and fat aggregates in larger clumps. MFGM components can also act as bioactive compounds:
- Sphingolipids are a special kind of lipids that play an integral part in cell membrane structure and make up about 25% of the myelin sheath in neural cells. Main function is to support the brain development of infants.
- Glycosylated lipids have a sugar molecule added to the lipid portion. Glycolipids function as anti-microbial agents and probiotics promoting the development of a healthy gut microbiome.
- Other MFGM lipids stimulate the maturation of the infant’s digestive tract.
Triglycerides, the main energy source for the infant, are stored inside the milk fat globular membrane. The fatty acid composition of those triglycerides is modified by the composition of the mother’s fat intake. For example if the mother eats fish and nuts her milk will contain more w-3 fatty acids which in turn promotes optimal brain development.
Human Milk Is Low in Protein and High in Carbohydrates Compared to Animal Milk
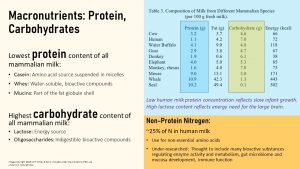
Human milk has the lowest protein content of all mammalian milks. The low protein content reflects the slow growth of human infants. While cows reach maturity after two years of life, humans grow and develop for 20 years. Of course the calf growing rapidly will need more protein that a human infant.
On the other hand, human milk has the highest carbohydrate content of all mammalian milks. This reflects the large brain of the human infant compared to animals. As you know brains prefer glucose as an energy source and an infant with a large brain will need more glucose than animals with a small brain.
Milk has three protein fractions:
- Casein is a generally slow digesting milk protein and delivers amino acid building blocks for infant growth and tissue maintenance. Casein makes up about 40% of mature milk protein and is suspended in micelles for improved digestion (increased surface for enzymatic digestion.)
- Whey is a fast digesting milk protein that makes up about 60% of mature milk protein. It is water-soluble and the primary function is not nutrition. Whey contains many bioactive components promoting immunity and digestive maturation.
- Mucins are the smallest fraction of milk proteins and contribute to the MFGM shell.
Human milk also contains a significant portion of non-protein nitrogen. This type of nitrogen acts as building blocks for non-essential amino acids. A few research studies have suggested that non-protein nitrogen serves other functions in enzyme regulation, bioactive component storage, gut microbiome development, mucosa development, and immune function but our understanding of the function of non-protein nitrogen is limited.
The carbohydrate content consists of two main fractions:
- Lactose, a disaccharide synthesized from one molecule of glucose and one molecule of galactose, serves as an secondary energy source.
- Oligosaccharides—carbohydrate chains of 3 – 10 monosaccharides—are indigestible and function as bioactive compounds maintaining the infant gut microbiome.
Bioactive Compounds From Human Milk Set Up Digestion and Immune System
Human milk is clearly ideal for the infant nutritionally. It delivers the perfect combination of nutrients and the amount is dialed in by the nursing infant. In the 1950s, 60s, and 70s this was the sole understanding of breast milk and it seemed easy to mimic this composition starting with cow milk. Scientists set out to mimic the human milk calling the result formula. The reasoning was that bottle feeding would make life easier for the new mother. Others can feed the infant (especially at night) so mothers can go back to work and are not all day long, all week long tied to the infant during the first year.
This understanding fueled the development of infant formula until research stumbled over surprising findings. Human milk contains an array of bioactive compounds that keep newborns and young infants healthy. Later scientists also started to understand that those bioactive compounds direct the development of a healthy gut microbiome and immune system that will last a life time.
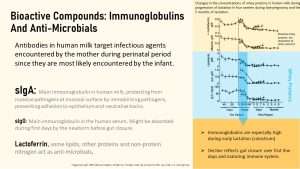
Looking at bioactive compounds in human milk, there are three major groups: Immunoglobulins and antimicrobials from protein, and a diverse group of oligosaccharides. Keep in mind that lipids also deliver anti-microbials.
Immunoglobulins and Antimicrobials
Infants are born with an immune system that needs to figure out first what are beneficial microbes and what are pathogens. This the reason why infants during the first months are very vulnerable to severe respiratory and gastrointestinal infections. At the end of the pregnancy the fetus receives some immunoglobulins via plancenta against the most common pathogens the mother experiences, but this first immunization doesn’t last too long.
After birth colostrum takes over. If you look at the graph above (light blue section to the right) you will see the high amounts of immunoglobulins the newborn receives via colostrum and also see that those amounts are declining to a lower level for mature milk. This makes it so important that every newborn receives colostrum if possible. As the infant’s gut microbiome develops and triggers a healthy immune system development milk producing glands reduce immune factor concentrations in the mature milk.
Going a little deeper:
- SIgG (secretory IgG) can be found in human milk in small quantities (in bovine milk it is the main immunoglobulin). SIgG is the main blood serum antibody and patrols the body on the lookout for pathogens. Scientists speculate that during the first few days before gut closure takes place (rapid reduction of epithelial permeability), sIgG can pass through those gaps and stimulate the infant’s immune system. As a consequence for example breastfed infants are less likely to have respiratory infections than formula fed infants.
- SIgA (secretory immunoglobulin A) is an important antibody that is secreted by mucosal immune cells of the mature gut mucosa to protect against common pathogens. The infant gut is immature and mucosal immune cells do not secrete IgA initially. SIgAs is produced by the mother against common pathogens in her environment and is secreted into the breast milk. Those sIgA protect the infant against pathogens hitching a ride in the milk. The secretory component protects the antibody against digestion—after all it is a protein—in the digestive tract. IgA and the other bioactive compounds work together to stimulate a healthy gut microbiome. That way the bioactive compounds teach the infant’s gut immune cells who is the enemy until the infant starts producing it’s own sIgA. More about that in the chapter about the gut microbiome development.
- Lactoferrin is also secreted by the mature gut epithelium, but initially not by the infant’s. The human milk lactoferrin works as an antimicrobial by trapping iron, an essential nutrient pathogens need to proliferate.
- Albumin and alpha-lactalbumin help with the transport and absorption of other nutrients.
Human Milk Oligosaccharides (HMO)

Human milk oligosaccharides (HMO) are a fascinating part of the human milk carbohydrates. The oligosaccharides might be indigestible for the infant but they play an essential role controlling the microbes that settle into the colon after birth. The essential part is that HMO ensure that very specific strains of bacteria can proliferate in the infant’s colon while others are basically starved to death. Oligosaccharides, with the help from immunoglobulins and antimicrobials, ensure that a healthy gut microbiome develops that in turn sets up a resilient, effective immune system. More about this later.
As you already know oligosaccharides from onions, beans, or whole grains are a favorite food for the mature gut microbiome. HMO have a controlling type A personality.
As you see above (light blue to the right) human milk contains an array of oligosaccharides. Interestingly, the HMO composition varies between women and it is thought that this variation is genetic.
Since human milk is the sole food the infant consumes during the first 4 to 6 months food for microbes is limited largely to HMO. Only bacteria strains that have the specific enzymes to digest the HMO will find enough food to proliferate. Sometimes leftovers from one bacterial strain’s digestion can be digested by a second strain. That way a very specific gut microbiome community is established in the human milk fed infant: Bifidobacterium and lactobacillus. The gut microbiome composition will never look that way again once human milk feeding stops or is supplemented with other foods. Formula fed infants will never develop this specific gut microbiome.
Oligosaccharides also pull double duty by serving as anti-adhesives that block microbial attachments to the gut epithelium and stimulate gut epithelial immune cells to improve immune response. Many pathogens, viruses, bacteria or parasites causing diarrhea, need to attach themselves to epithelial cells to proliferate. They attach to glycans on the cell surface of epithelial cells. HMOs mimic those glycans and pathogens attach to the HMOs instead and getting excreted in the feces.
Only 1% of oligosaccharides are absorbed and excreted unchanged in the urine. The remainder is either digested by the gut microbiome or excreted in the feces of the infant. It’s not clear if HMO have more functions than feeding the gut microbiome.
Is Breastfeeding All Work, No Benefits For the Mother?
From sleepless nights to sore nipples to finding a room to pump that isn’t a bathroom at work, breastfeeding seems stressful and often benefits seemed small compared to the stress. The benefits for the infant are truly amazing but mothers should keep in mind that breastfeeding has benefits for her too:
•Rapid shrinking of the uterus and reduced blood loss post partum due to the breastfeeding hormones
•Less blood loss due to suppression of menstruation as long as breastfeeding continues through night
•Faster return to pre-pregnancy weight due to substantial increased energy needs
•Decreased risk for breast, endometrial and ovarian cancer (negatively correlated with total months of breastfeeding)
•Convenient, cost free, less missed work, environmentally friendly
When Breastfeeding Is Not Perfect

While we have highlighted many important benefits of human milk in infant development, there are also some situations in which breastfeeding is not advised. It was mentioned a few times above that the mother’s milk composition is highly reflective of her own dietary composition. This means that if the mother is deficient in certain nutrients, then the infant could also become deficient. Eating a balanced diet during lactation such as MyPlate, Mediterranean, vegatrian will supply all nutrients needed.
Some common deficiencies found in infants to pay special attention to are:
- Vitamin B12 deficiency: Since only animal based foods provide vitamin B12 vegan mothers run the risk of producing breastmilk low in or devoid of vitamin B12. Infants from vegan mother’s tend to be born with low B12 stores if the mother doesn’t supplement vitamin B12 (supplements or fortified foods) during pregnancy. During breastfeeding the infant gradually becomes vitamin B12 deficient leading to impaired, sometimes irreversible neurological development. It is essential that nursing vegans supplement vitamin B12.
- Vitamin D deficiency: Newborns and young infants have a very sensitive skin and burn easily. Therefore it is recommended that infants are kept in the shade where they don’t produce too much vitamin D. Since breastmilk is low in vitamin D, rickets a softening or weakening of bones can develop especially in infants born in the winter in Northern latitudes. Mothers are advised to supplement breastfeeding with vitamin D drops as a preventative measure.
- Infants are born with very low vitamin K stores. During the first weeks the infant consumes only small amounts of milk and lacks initially a gut microbiome that will later produce vitamin K. Once milk volumes increase and vitamin K production by the gut microbiome starts, the vitamin K intake is sufficient. You realize that there is a gap after birth when vitamin K deficiency can develop. In the past infants were at risk for hemorrhage disease due to vitamin K deficiency which could lead to dreaded bleeding in the brain. There is an easy fix and today newborns can receive a recommended vitamin K shot right after birth. Since this practice started vitamin K deficiency disease is almost unheard of.
Lastly, some viral diseases such as HIV or Hepatitis B can be transmitted through breastmilk and women with those diseases are advised against breastfeeding.
Interested In More Information?
Practical Information: La Leche League https://lllusa.org/
https://www.cdc.gov/breastfeeding/index.htm
Editor: Sydney Christensen, Eric Hanzel
NUTR251 Contributors:
- Spring 2020: Rose Davidson, Cameron Hucke, Brett Freitag, Melanie Nissen, Amelia Johnson, Caroline Leibel, Kendyl Heuertz, Eli Havekost, Kyle Dawson, Ellen Koch, Keeley Hagge, Allison Aden, Dario Henry, Grant Young, Max Kleinschmit
- Fall 2020: Clare Caraghar, Carly Schwager, Bryson Krull, Miles Judson, Peyton Hainline


Feedback/Errata
16 Responses to Human Milk Is More Than Nutrition For Infants