18 Formula Is Not a Protein Shake For Infants
Sabine Zempleni; Eric Hanzel; and Sydney Christensen

The recommendations for feeding an infant during the first year are clear: If possible infants should be fed exclusively with human milk for the first 4 months, ideally during the first 6 months. Then parents should keep feeding human milk while transitioning to family meals. Why is infant formula then such a thriving business?
Nursing an infant was once a natural process. Older women shared their wealth of experience and knowledge how to nurse, and soon the new mother became a nursing pro. During the time of breastfeeding, the mother and child were together almost all the time. This system was essential for the survival of the infant. If a mother did not produce enough milk, a wet nurse had to be found who fed the infant along with her own infant. Upper class women often did not nurse their own children. They either employed a wet nurse or during slavery a female slave was forced to nurse the owner’s infant.
During the 19th century two scientific advances laid the ground work for infant formula. Scientists discovered how to analyze energy content and macro-nutrients in food. The second discovery was the understanding of bacterial growth in food and how to prevent it. Pasteurization was invented. The first formula was invented in 1865 by Justus Liebig, a professor at the University of Giessen in Germany (coincidentally I graduated from the Justus Liebig University in Giessen.) Liebig’s soluble food for babies was a powder made from cow’s milk, wheat flour, malt flour, and potassium bicarbonate. Slowly over time the modern infant formula we know today was developed.
In the 1960s, aggressive marketing campaigns by infant formula manufacturers changed how infants were fed and breastfeeding rates plummeted. Women were told that formula feeding was just as good as breastfeeding but easier. Women could stay in the work force or have a break from infant care. As a consequence, a generation of women never nursed. When public health professionals started promoting breastfeeding in the 70s and 80s this generational knowledge was missing. Today, midwifes and lactation consultant are working on reviving this knowledge.
You Will Learn:
- Most US mothers start out breast feeding after but many barriers prevent them from continuing to breastfeed.
- The formula industry is a 3.65 Billion market in the US with a confusing variety of formulas to choose from
- Formula is not just cow’s milk plus added nutrients
- Cow’s milk-based formula is the go-to formula for most infants
- Hypoallergenic formula is used when infants are allergic to cow’s milk
- Soy-based formula was used in the past in case of allergies but soy is also a potent allergen
- Formulas are not protein shakes: While formulas vary slightly in composition, they all have to follow strict regulations:
- The nutrient composition of formula must adhere to FDA guidelines
- Formula must support adequate growth
- Formula must meet safety and quality control guidelines
- Human milk and formula are close but important differences persist:
- Formulas mimic the nutrient composition of human milk well
- Many bioactive components of human milk are still elusive
- Formula fed infants have a completely different gut microbiome than breastfed infants
- Even If breastfeeding is sometimes hard, formula feeding should only be considered if breast feeding is not possible
- Colic and practicality are often front and center when choosing between breastfeeding and formula
- If a mother doesn’t nurse food safety rules become important to protect the vulnerable infant
Most US Mothers Start Out Breast Feeding After Birth But Many Barriers Prevent Them From Continuing to Breastfeed

The good news first, in the United States, a large majority—over 80 %—of mothers start out exclusively breastfeeding after birth which means the majority of infants receives the immunological and developmental benefits of colostrum. After that the breast feeding rate declines fast. Only a quarter of American mothers make it to the recommended 6-month mark of exclusive breastfeeding. Many infnats are still partially breastfed though.
There are also clear disparities. Breastfeeding rates are higher in the North-Central and North-West US and lower in parts of the Southern US. Educated women are more likely to breastfeed and women of color less likely.
Despite their efforts there are many reasons why a mother may choose formula feeding over breastmilk. Here are a few:
- Access: Even if the woman has access to a lactation consultant some mothers are not able to produce enough breast milk. This can happen any time during breast feeding. As you know from the last chapter, feeling under pressure and being stressed disrupt for example the hormonal system.
- Physiology: Women with obesity are at a higher risk not being able to nurse or produce less milk. Since around 40 % of women during the reproductive years are obese in the US, this affects many women. Newer studies also show that the milk might have a different fatty acid composition if the nursing mother is obese. Some mothers develop mastitis, a painful inflammation of the breast, and cannot nurse at least temporarily until the infection has cleared up.
- Health policy: Not everyone has fully paid maternity leave in the US. It all depends on the state, the size of the company, and how long the mother has worked for the company. Ideally, the new mother might get 12 weeks of paid leave. This is the shortest maternity leave for affluent countries.
- Health Policy: Working mothers have to pump milk 3 to 4 times during the eight hour work day to maintain milk production. Each session takes between 20 to 30 minutes. While there are laws in place to allow for pumping, hourly paid worker might not be paid during those breaks or the work environment might be hostile to pumping. Many smaller employers do not provide a private room and women are forced to pump in closets or bathrooms.
- Personal: The mother does not have sufficient support from partner or family and feels overwhelmed. Breastfeeding during the night might leave the parents too tired for the work day.
- Education: The parents are not sufficiently educated about the benefits of breastfeeding or are misinformed.
The Formula Industry Is a Highly Competitive 3.65 Billion Market With a Confusing Variety of Formulas to Choose From
Since the the start of formula feeding in the early 20th century formula has come a long way. Starting out as a nutrient powder to add to diluted cow’s milk, formula is today a complicated food product that mimics breastmilk as closely as possible.
When the parents decide that it’s time to make the switch to formula, there are confusingly many formula brands on the market. The best-known brands are Similac (Abbott Nutrition), Enfamil (Mead Johnson), and Gerber (Nestle). Additionally, there are store brands and smaller organic brands. Each of those brands carry not just one formula, but a line-up for different age stages and even several formulas for each age stage.
The marketing strategy is to give parents a choice, suggesting that parents can find the best formula for their infant. Marketing strategies aim first at hospitals where the mother gives birth or pediatrician offices. Hospitals and pediatricians are supposed to hand out baby bags, bottles, nipples, samples, and brochures with coupons for the expensive formula. The marketing goal is that the parents feel that the formula has their pediatrician’s seal of approval. Even if the parents to breastfeed, the merchandise serves as a reminder to the new parents that they can switch to formula at all times. This initial targeting is followed up by ubiquitous ads promising a good night of sleep, optimal brain development, and less colicky babies. Aggressive marketing is not surprising since the infant formula market was in 2019 a 3.65 billion dollar market.
Formula is Not Just Cow’s Milk Plus Added Nutrients
Recall from the last chapter that breastmilk basically has a mind of its own. It can adjust nutrient composition from the bioactive colostrum to the carbohydrate rich mature milk which adapts to the individual needs of the infant. Unfortunately, formula does not have the same autonomous function as breastmilk. Once parents choose a formula the infant will receive the same nutrient composition for each meal every day. In chapter 21 Developing Good Taste you will also learn that breastmilk undergoes subtle flavor changes depending on what the mother is eating. Formula has a consitent flavor and it is thought that this impacts taste development in the infant.
As mentioned, there are many options on the market we will not explore in detail. The three basic options to choose from are: Cow’s milk-based, soy-based, and hypoallergenic formula. All three provide similar nutrient compositions but contain different ingredients.

Cow’s Milk-Based Formula
Cow’s milk-based formula is usually the go-to formula for most parents. At first glance, it may just seem like an enhanced cow’s milk but a closer look at the nutrition label and one can see that cow’s milk formula is not whole milk plus/minus nutrients. Synthetic formulas are designed to mimic the macro- and micronutrient composition of breast milk.
- The basis is the nonfat cow’s milk. Since cow’s milk contains much less lactose than human milk, the first step is to add more simple carbohydrates. Some formulas add those carbohydrates in form of lactose and others as corn syrup. The reasoning behind the corn syrup is that some colicky infants are sensitive to lactose. Corn syrup (a mix of the mono-saccharides glucose and fructose) seems to be easier digestible.
- Cow’s milk contains predominantly casein. Human milk contains more whey protein. Therefore, protein is reduced overall and whey protein is added. This way the high protein content of cow’s milk can be reduced by increasing protein quality.
- A variety of vegetable oils is used to mimic the fatty acid profile of human milk.
- Vitamins and minerals are added in recommended amounts.
- Some of the bioactive ingredients found in human milk are added.
It is not necessary to memorize the ingredient list, but use the infographic above to familiarize yourself with nutrition labels on formulas.
Soy Based Formula
In the past soy based formulas were the go-to formula when infants either had a diagnosed allergy to cow’s milk protein or allergies were running in the family. It became clear quickly that soy protein has the same high allergy potential as cow’s milk protein. Today hyper-allergenic formulas are recommended instead. Why are soy based formulas still on the market? Hyper-allergenic formulas taste bitter and some infants will not tolerate that. Vegan mothers who can’t breast feed might also opt for soy-based formulas. Desperate parents of colicky infants might give it a try. In short, soy-based formulas are still around.
This type of formula is plant based as the name suggests but very different than the soy milk you find in the store. Producers start with soy protein—the only plant protein that is a complete protein—and add nutrients. The first ingredients listed on soy-based formula are:
- Corn syrup solids/sucrose
- Soy protein isolate
- Variety of vegetable oils
Just underneath, you’ll find again the additional vitamins, minerals, and bioactive compounds required in formula.
Hypoallergenic Formulas
An alternative for infants with milk allergies (or soy allergies) are hypoallergenic formulas also known as protein hydrolysate formula. This kind of formula uses cow’s milk, but the protein is hydrolyzed and broken down into peptides. Hypoallergenic formulas can have a higher or lower degree of protein hydrolyzation. Hydrolyzing protein into short peptide fragments reduces the allergy potential. The higher the degree of hydrolyzation the lower the allergy potential.
The infant might not be a fan because hydrolyzed protein tastes bitter. Therefore newborns get used to it easier than older infants who already have tasted the non-bitter, sweet original. In addition, the production of hypoallergenic formula is much more expensive.
Hypoallergenic formula should only be used on recommendation of the pediatrician. It is important to know that this formula will come with no added nutritional benefits, but with worse taste and higher cost. Therefore, it should only be used when medically indicated.
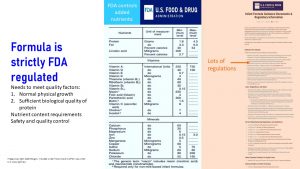
Formulas Are Not Protein Shakes: While Formulas Vary, They all Have to Follow Strict Regulations
Formula is not produced like protein powders. Protein powders are considered “foods” and not scientifically tested before going on the market. There is also no requirement for quality control. This is up to the individual producer. Protein powder manufacturers can also tweak their recipe as long as the ingredients are food-based. Only if the protein powder is on the market and complaints arrive will the FDA investigate. It seems common sense that infants should not be guinea pigs.
Formula manufacturers have to conduct studies to prove that any new formula is safe for infants. Even tweaking an existing formula recipe, such as adding oligosaccharides, involves many scientific studies. Study results have to be presented to the FDA which approves the change or doesn’t. In addition, once a formula is approved by the FDA, production involves strict quality control so the powder contains what it is supposed to contain (unlike protein powders and other supplements.)
Manufactures have to meet strict guidelines and have to prove that the formula:
- Allows for normal physiological growth of the infant comparable to breastfed infants. Not too fast, not too slow.
- Contains sufficient amounts of biologically adequate protein with a protein content similar to breastmilk.
- Contains exact amounts (in some cases a range) of macro- and micronutrients.
- Meets safety and quality control guidelines.
Since these guidelines required every manufacturer to produce a formula with almost identical nutrient composition, manufacturers invest in research to come up with small differences they can advertise. Formula enhancements include the addition of prebiotics, probiotics, extra omega-3 fatty acids, or oligosaccharides. The competitive advertising has not only the aim to draw parents away from breastfeeding, but also from the competing brands. The result is a confusing formula market for parents. Parents are not equipped to make this decision on their own, but should talk to a pediatrician or PA.
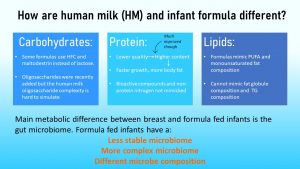
Human Milk and Formula are Close but Important Differences Persist
Despite research efforts formula manufacturers are still unable to match the benefits of breastmilk. So, what continues to make these two so different? The answer is simple – complexity. Formula has yet to achieve the natural complexity of nutrients and bioactive compounds found in breastmilk and we will explore how this impacts an infants growth and metabolism.
The Carbohydrates
As mentioned in the previous section, all formulas are required to maintain a specified composition of macronutrients, but formula does not necessarily only contain lactose. During the first days of life, not only lactase, but also amylase activity increases in the infant’s gut. This makes it possible to replace lactose with sucrose or maltodextrines. The manufacturers argue (and advertise) that less lactose means less colic. Keep in mind that corn-syrup is cheaper than other sugars.
We also discussed in the previous chapter that human milk contains insanely complex oligosaccharides that promote a microbiome that is only seen in breastfed infants. Formula manufacturers are on a scientific hunt to identify as many oligosaccharides as possible, figure out what bacteria of the microbiome are promoted, and find a way to synthesize these oligosaccharides.
In recent years, formula manufacturers were able to synthesize a few oligosaccharides and add them to the formula. But, those oligosaccharides while heavily advertised are not remotely close to promoting the gut microbiome that breastfeeding allows.
The Proteins
The formulas of the 1970s and 80s had a much higher protein content than breast milk to make up for the lower protein quality. These high-protein formulas were not only less than ideal for immature kidney function, but infants had an increased body fat content and higher growth rate than breastfed infants. Studies following those infants showed that those high-protein formulas increased the risk for obesity and chronic diseases down the road. Reducing the amount of protein by increasing protein quality slowed the growth of formula-fed infants down to a more comparable rate to breastfed infants. Still, formula-fed infants have a higher risk for obesity and non-communicable diseases down the road.
Similarly to carbohydrates, the protein components found in formula fail to mimic the bioactive whey proteins and non-protein nitrogen in human milk. Recall that bioactive compounds and non-protein nitrogen support the development of a healthy gastrointestinal and immune system. Antimicrobial proteins also protect infants from pathogens. Breastfed infants tend to have less diarrhea, respiratory illness, ear infection, allergies and even a lower prevalence of SIDS (sudden infant death) than formula-fed infants.
The Fats
You probably already know what’s coming. Formula fats mimic the fatty acid composition of human milk well but that’s where it ends.
The human milk fat globule and triglyceride composition, on what carbon individual fatty acids are linked, is designed for ideal digestion. Formula fat is less easy to digest and absorb. Components of the fat globule shell, such as sphingolipids, are crucial for optimal brain development, immunity, and gut maturation.
The Gut Microbiome (Mini-Preview)
Overall, formula composition made huge improvements and mimics the nutrient composition of human breastmilk well. One of the main problems formula manufacturers need to solve is the promotion of the ideal gut microbiome. Gut microbiome development (see The Road to a Healthy Gut Microbiome) is closely connected to immune system development. During infancy, gut microbiota promoted by formula are less stable, composed from different microbes and much more complex than the simple, unique breast milk microbiome.
While the research is still brand-new, scientists are worried that these differences in gut microbiome composition are factors promoting obesity and chronic diseases. Even if it seems sometimes hard to feed an infant with breastmilk, research today shows us that it is very much worth it in the long run.
Even If Breastfeeding Is Sometimes Hard, Formula Feeding Should Only be Considered if Breast Feeding is Not Possible
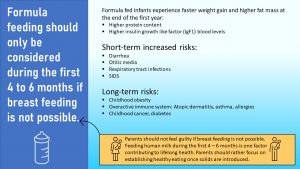
Aside of the huge impact on the gut microbiome, formula feeding comes with additional risks. Some are short-term and other impact the child long after formula feeding has stopped.
Short-Term Risks
The short-term risks are mostly due to the lack of anti-microbial, bioactive substances the breastmilk provides. Oligosaccharides, mucins, some whey proteins, and some lipids act as antimicrobials. They prevent the pathogens from attaching to the gut epithelium and neutralize pathogen toxins.
In addition, human milk contains antibodies, sIgA and sIgG, the mother produces in response to the environment she is living in. All this together promotes a healthy gut microbiome and the development of an efficient immune system.
Lack of those bioactive nutrients in formula leads to a higher risk for:
- Diarrhea
- Otitis media
- Respiratory Tract Infection
- SIDS
Long-Term Risk
Epidemiological research is showing for decades that children who were predominantly formula fed as infants are more likely to have the following conditions:
- Childhood obesity
- Atopic dermatitis, asthma, and allergies
- Childhood cancer and diabetes
For a long time it was unclear why this connection was found. Newer research seems to be on track explaining the physiological mechanisms. It is thought that the gut microbiome and immune system are established differently in formula fed infants. While other factors such as birth mode, timing and type of solids, family meal, and living environment play a role too, it seems that formula feeding is one of the contributing factors to a less desirable microbiome composition.
In consequence, the distinctly different early microbiome leads to the development of a less resilient, sometimes overactive immune system. It’s important to note that research is still ongoing and many other factors affect the overall development and immune function of an infant as well. With this information, we can see just how big of a role breastfeeding plays into the health of the infant, child, and later adult.
Parents should not feel guilty if breast feeding is not possible. Feeding human milk during the first 4 – 6 months is one factor contributing to lifelong health. Parents should rather focus on establishing healthy eating once solids are introduced.
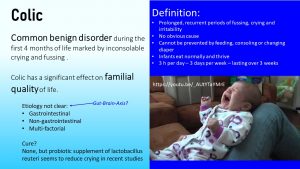
Colic and Practicality are Often Front and Center When Choosing Between Breastfeeding and Formula
When we think about parenthood we think about blissful parents cuddling their newborn baby. This bubble of happiness is often pierced if the sweet infant turns into a raging, colicky baby. Nights of taking turns to carry the inconsolable infant around the house turn blissful parents into sleep deprived zombies who have problems functioning during the day. What is colic?
Here is a great YouTube video demonstrating the stress parents are experiencing having a colicky infant: “Here’s the non-sugar coated, raw reality of colic. This is my daughter at almost 4 weeks old and just a small sample of how we spent the first few months of her life. Damaging, life altering, heart breaking experience. There was absolutely nothing we could do to sooth her…nothing.” from MyBabyHasColic
Physicians and scientists have some guesses, but it is not really clear what a colic is physiologically. Hypotheses include a GI system with an immature motility, a lack of coordination between digestive processes and motility, or an under-developed gut microbiome. Other non-gastrointestinal factors such as neurological immaturity are also discussed.
To parents it seems that something is badly wrong with their infant, but colic is a common benign infant disorder that occurs during the first four months of life marked by excessive amounts of crying and fussing. Colic is diagnosed if episodes of crying and fussing occur for more than three hours a day, three or more days a week, and persist for more than three weeks.
The American Pregnancy Association suggests that all babies experience some level of colicky behavior but only about 20 – 25% of infants are diagnosed with colic. While the colicky baby is healthy, the situation can have a significant impact on the family’s quality of life. At the moment, there is no official cure for colic so parents must endure the natural course of things. Limited research has shown that supplementation with probiotics could reduce the severity of colics and that’s why formula manufacturers add it to formulas and advertise it.
If a Mother Doesn’t Nurse Food Safety Rules Become Important to Protect the Vulnerable Infant
When it comes to food safety nothing is easier than nursing an infant. The milk is there when needed, temperature is right, and the antimicrobial bioactive nutrients squash potential pathogens. Nursed babies, drinking directly from the breast, have rarely GI infections which can put the infant at risk for dehydration.
Once the parents switch to feeding pumped breastmilk or formula, the parents must follow a set of food safety rules.

Even then pumped and stored breastmilk has its advantages. Breastmilk contains antimicrobials, secretory IgG, and live white blood cells. This allows for storage at room temperature for up to 8 hours (I still would store the breastmilk in the fridge as soon as possible or freezer if there is a surplus.)
During the first three months it is essential that all equipment coming in contact with breastmilk—pump, bottle, nipples, storage containers—is sterilized by boiling it for 5 minutes in water and then removing the items with tongues. After the infant is older than 3 months washing items in the dishwasher or in hot soapy water will be sufficient.
Formula does not contain antimicrobials, so, the list of food safety rules expands. Have a look: The CDC webpage gives detailed instructions how to wash infant feeding utensils.
Other important safety rules, in addition to cleaning equipment, when feeding formula are:
- Ideally prepare only one serving of formula. Since it is a pain to get up at night to prepare a bottle or get liquid formula from the fridge, parents like to skip this safety rule. An alternative approach might be to keep the boiled and cooled down water in the bottle and add the pre-measured powder when it is time to feed. Bacteria do not grow in boiled water kept in a sterilized bottle.
- Once the formula is prepared, it needs to be refrigerated iimediately and used within 24 hours. Same goes for open, premixed formula No keeping the bottle with mixed formula in the holder of the stroller on an outing or on the bedside table during the night, or mixing the formula supply for several days.
- Leftover bottles need to be discarded since the suckling infant mixed the milk with enzymes and microbes from the mouth. These microbes will start the process of digesting the formula spoiling the milk even in the fridge. This safety rule also applies to leftover breastmilk.
- Check that the water supply is safe especially when using well water or living in a rural area. Water must have a nitrogen concentration under 10 mg/L. High nitrogen concentrations won’t harm children over one year of age or adults but can lead to life-threatening blue-baby syndrome.
- Don’t boil the water for a long time. One minute is enough to kill off pathogens. Water dissipates during prolonged boil times and the mineral content increases. Remember immature kidneys? PRSL? Prolonged boiling concentrates minerals in the water and adds to the PRSL of the formula. Let water cool down before mixing with powder.
- Don’t microwave formula or breastmilk. Microwaving creates hot spots in the milk and infants got badly burned drinking microwaved formula that was not shaken properly.
Interested In More Information?
- CDC: Breastfeeding information and Formula Feeding Information
- Food safety: Infants and Under 5 years old
- Healthy People 2030: https://health.gov/healthypeople/objectives-and-data/browse-objectives/infants
- Baby Friendly USA
Editors: Sydney Christensen, Eric Hanzel
NUTR251 Contributors:
- Spring 2020: Miranda Haverdink, Caleb Licking, Caroline Leibel, Danae McKenzie, Jenna Junker, Shane Rapp, Alondra Iturbide, Kennedie Engles, Eli Havekost, Haley Jensen
- Fall 2020: Megan Appelt, Morgan McCain, Peyton Hainline, Shalin Bhakta
Protein that contains all essential amino acids in adequate amounts to synthesize human protein. Other plant milk sources such as almond, oats or cashew, contain incomplete proteins and are not adequate as an infant milk. Therefore the only plant-based infant formula is based on soy.
The use of nitrate-contaminated drinking water to prepare infant formula is a well-known risk factor for infant methemoglobinemia (blue-baby syndrome). Nitrate can also stem from excessive feeding of nitrate-rich vegetables such as beets. Affected infants develop a peculiar blue-gray skin color and may become irritable or lethargic, depending on the severity of their condition. The condition can progress rapidly to cause coma and death if it is not recognized and treated appropriately. Inants are born with fetal hemoglobin that can bind nitrate and block therefore the transport of oxygen. Fetal hemoglobin is replaced by hemoglobin by 6 to 12 months.
Potential Renal Solute Load:
Amount of Na, K, P, Cl, and N (from protein and non-protein N)


Feedback/Errata