4 Hypertension Is a Silent, Often Overlooked Disease
Gabi Ziegler and Sabine Zempleni

How do you feel when you have hypertension? Normal, and that is a major problem. Most people with mild to moderate hypertension feel completely normal and this means that their high blood pressure will silently damage blood vessels sometimes over years until the blood pressure is checked at the physician’s office.
Blood circulating with high pressure through the cardiovascular system pushes against blood vessel walls. The blood vessels react to the increased pressure by thickening the muscles embedded in the blood vessel walls. Thicker walls become stiffer and decrease the ability of the blood vessels to cushion normal blood pressure spikes due to stress or exercise for example. This is called increased vascular resistance.
While you feel normal the increasing vascular resistance increases blood pressure further—in short hypertension is a self-amplifying condition once the process has started. Over time the blood vessels become damaged. This contributes to the development of atherosclerosis and damage to target organs resulting in kidney dysfunction, declining cognition, stroke and damage to eyes.
Lifestyle interventions can reverse hypertension but are only effective in reversing mild hypertension and not in controlling high blood pressure. This makes it so important to identify individuals at risk, diagnose early, and start lifestyle intervention when the hypertension is still mild.
Before going into the details first review what you already learned in previous courses:

You Will Learn:
- Hypertension is the chronic disease with the highest prevalence in the USA.
- Non-modifiable risk factors are age and genetics. The main modifiable risk factors are obesity, a Western lifestyle, alcohol abuse and diabetes.
- Blood pressure is regulated by the autonomic nervous system and the renin angiotensin aldosterone system (RAAS).
- Obesity leads to a combination of increased cardiac output, excessive sympathetic activation and RAAS overactivity: Blood pressure increases.
- Hypertension is a self-amplifying condition getting progressively worse due to damage to blood vessels and target organs such as kidneys and heart.
- Since blood pressure due to obesity is multifactorial it is often drug resistant. First line of treatment is therefore weight loss. The DASH diet and increased physical activity have been shown to be effective in reversing elevated blood pressure and moderate hypertension.
Hypertension Is the Most Common Chronic Disease in the USA
In 2017, the American College of Cardiology and the American Heart Association re-defined hypertension after evaluating recent research. This reserch indicated that the correlation between between blood pressure and the risk increase for CVD starts already when the blood pressure crossed the normal threshold of 120/80. The new recommendations inserted a new category, evelated blood pressure, and lowered the diagnostic criterium for hypertension from 140/80 to 130/80 mm Hg. Thie is the reason why prevalence increased after this change by around 10 %. The goal of this new recommendation was not to scare Americans but to identify people in the process of starting the self-amplifying cycle of hypertension earlier.
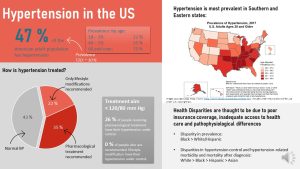
Using the new 2017 definition of hypertension nearly half of US Americans were considered hypertensive in 2018. The prevalence of 47 % is an average over all adults though. By the time Americans reach age 60 most people (~75 %) have developed hypertension in the US.
Hypertension was always a prevalent disease especially in higher age groups. From 1999 to 2010 prevalence of hypertension declined from 47 % to 42% but over the last decade this progress has been reversed. Data from 2020 show that the prevalence is right back at 47 %.
Even more concerning is the fact that many US Americans diagnosed with high blood pressure are not able to successfully manage their blood pressure with medication and lifestyle changes.
The average prevalences does not tell the full story. Hypertension is more common in the Southern and Eastern United States as the map above shows. Keep in mind that the prevalences from this map look lower because the data is self-reported and therefore people who are not aware that they have hypertension are missing.
When we analyze the CDC data for hypertension further there are several more disparities aside of the geographic variation:
- More men than women have hypertension. Part of this observation is that women have a moderate protection against hypertension before menopause by the hormone estrogen.
- In 2017 and 2018 high blood pressure was most prevalent in Black adults with 57 %. White and Hispanic adults have a much lower prevalence of 44. For Asian Americans the situation is more complex. While Chinese Americans have a lower prevalence than white Americans, Filipinos for example have a high prevalence similar to Black Americans.
- Once hypertension is diagnosed blood pressure control is not great. White adults are more successful than Black adults while Hispanic and Asian adults do worst.
The reasearch evaluating the reasons for those health disparieties is just starting. Scientists assume that poor insurance coverage (f.e. high deductibles) and inadequate health care access (no time, transportation, cultural factors) are in part to blame. Recent research also dicusses the fact that there might be pathophysiological differences in blood pressure regulation in Black Americans while pharmacological treatment was developed mostly based on studies including white Americans.
The Main Risk Factors For Developing Hypertension Are Age And Obesity
This data raises the question how hypertension starts in the first place and why we saw another uptick in prevalence during the last ten years. Some of the risk factors for hypertension are non-modifiable while others can be modified.
The non-modifiable risk factors are age, genetic pre-disposition and gender.
While the effects of an unhealthy diet and sedentary, stressful lifestyle damage blood vessels during the course of the life, age in itself is one of the major risk factors for hypertension. This means that many adults with a perfectly healthy lifestyle will develop hypertension in higher age. The physiological mechanisms are not fully understood, but scientists think that the increasing blood pressure with age is due to changes in hormonal regulation and physiological stiffening of arteries.
Women tend to have a lower blood pressure than men until they reach menopause when women catch up to men. Scientists also suspect that some people have a somehwhat different way to regulate blood pressure. For exampl the blood pressure declines at night when you are sleeping. For some people this decline is not as pronounced contributing the self-amplification—I’ll explain later—of hypertension.
Risk factors that can be modified include obesity, high sodium intake, low fruit and vegetable intake, low physical activity, stress and excessive alcohol consumption.
Aside of age, obesity is the second major risk factor for hypertension and the single most important modifiable risk factor for hypertension. Epidemiological studies show that 65 – 78 % of the risk for primary hypertension might be due to obesity. In addition, new research suggests that hypertension due to obesity is aggravating damage to the heart potentially leading to heart failure.
Diet and lifestyle are considered to have an important place in the prevention of high blood pressure. A healthy lifestyle prevents early onset of hypertension and prevents mild hypertension from becoming severe. Frustratingly, diet and lifestyle treatment tend not to be very efficient in reversing hypertension or managing high blood pressure.
High fruit and vegetable consumption supplies ample amounts of potassium and most American adults are not even close to meeting the fruit and vegetable recommendations. Potassium tends to reduce blood pressure while high sodium intake from processed foods tends to elevate the blood pressure. A diet high in fresh plant-based foods and low in processed foods such as the DASH (dietary approaches to stop hypertension) diet has been shown to reduce the risk for severe hypertension.
Interestingly, regular physical activity and exercise lowers blood pressure by first elevating it temporarily. In order to deliver more oxygen during exercise to the muscle heart beat and stroke volume are increase which raises the blood pressure. You can imagine this temporary raise in blood pressure like a massage for the blood vessel walls. The pressure against the blood vessel walls generates shear forces triggering the blood vessel walls to secrete nitric oxid (NO) which in turn relaxes the smooth muscles in the arterial walls. Relaxed blood vessels result in lower blood pressure.
Myth or Fact?
You might have heard about the recommendation to eat foods containing lots of nitrates such as beet root juice or leafy greens to relax blood vessels and lower blood pressure. The nitrate is converted partially into nitric oxid by the bacteria in the gut which is absorbed. Hypothetically, increased nitric oxid blood levels relaxe blood vessels, reducing vascular resistance, and in turn reducing blood pressure. Scientists are intrigued by this and are researching the properties of these foods as a way to lower blood pressure and increase circulation. So far the effects seen are small though.
Caffeine causes a transient BP spike for up to three hours after consumption. It is not fully clear why. Increase in heart rate or the diuretic effect of caffeine are discussed. Frequent consumption of caffeine results in the development of a caffeine tolerance. The post-caffeine spike becomes less marked. Therefore, long-term caffeine consumption does not have much of an effect on BP or is a risk factor for hypertension.
Alcohol raises the blood pressure briefly due to diuretic effect (=long bathroom lines at the bars). The body responds to the loss of fluid by starting fluid conservation measures which increases blood pressure. Once the effect of alcohol wears off the blood pressure will go back to normal.
A greater issue than an occasional glass of wine is regular binge drinking (more than 3 standard drinks on one occasion). Regular binge drinking also comes with the transient blood pressure increase, but additionally tends to increase the activity of the sympathetic nervous system over time (more about that later.) A higher level of sympathetic nervous system activity means higher blood pressure.
In summary, there are two standout factors that spike the risk for hypertension: Age and obesity. Since age is a non-modifiable risk factor, you will explore how obesity is connected to hypertension during the remaining chapter.
The Blood Pressure Is Regulated By The Autonomic Nervous System and RAAS
In order to understand the connection between obesity and hypertension you will need to understand how blood pressure is regulated.
Two major metabolic systems are involved in blood pressure regulation: The autonomic nervous system regulates short-term blood pressure fluctuations and the endocrine RAAS system takes care of the long-term regulation. Both systems change when weight increases.
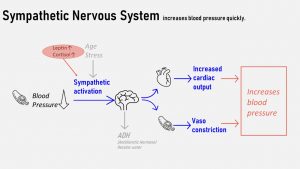
The autonomic nervous system is the part of the nervous system that runs in the background to regulate essential body functions. It has two antagonistic arms, the sympathetic and parasympathetic arm. In general, the sympathetic nervous system excites bodily functions while the parasympathetic nervous system calms down those functions.
Baroreceptors located in arteries monitor the pressure against the receptors and activate either the sympathetic or parasympathetic arm to adjust cardiac output and vascular resistance. The figure above shows the sympathetic arm because that’s the one affected by obesity.
When the baroreceptors detect that the blood pressure is too low, they signal to the corresponding regulatory center in the brain. The sympathetic nervous system is activated and nerve impulses increase the cardiac output by increasing the heart rate and volume expelled with each beat. The same nerves also signal to the smooth muscles of the peripheral arteries to contract more. This signal leads to a narrower blood vessel lumen. Pushing more fluid through a narrower vessel increases the pressure.
If the blood pressure is too high this is also detected by the baroreceptors and the parasympathetic nervous system calms cardiac output and relaxes smooth muscles in the blood vessels.
If the sympathetic nervous system is activated for example by stress it will also increase blood pressure. With age the sympathetic nervous system tends to be easier activated and may stay on a higher activation level. It is thought that this physiological change is one of the reasons why blood pressure is higher even in healthy aging individuals.
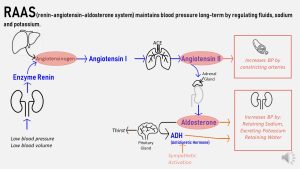
The renin-angiotensin-aldosterone system (RAAS) regulates blood pressure log-term by regulating the fluid balance. There are three components to this regulation: fluid, sodium and potassium balance.
- Renin, an enzyme, is secreted from the kidneys when blood pressure is low or blood volume is low for example in dehydration. The system is also activated to retain sodium or excrete excessive potassium.
- The circulating renin catalyzes the conversion of angiotensinogen to angiotensin I. Inactive angiotensinogen is secreted from the liver and circulates in the blood stream.
- Angiotensin I travels the blood stream now until it reaches the lungs where another enzyme, ACE, catalyzes the conversion into the active hormone angiotensin II.
- Angiotensin II prompts the peripheral blood vessel muscles to constrict. This raises the blood pressure.
- Angiotensin II also acts on the adrenal gland on top of the kidneys which secretes aldosterone. Aldosterone starts retaining sodium and fluid while excreting potassium. This mechanism increases fluid in the circulation and blood pressure.
- Aldosterone also acts on the brain causing thirst and releasing another hormone from the pituitary gland, antidiuretic hormone (ADH). ADH also acts on the kidneys to retain water, increasing the blood pressure.
The autonomic nervous system and the RAAS system are not two separat regulatory systems but are connected. When baroreceptors detect low BP and activate the sympathetic nervous system it will also prompt a secretion of the hormone aldosterone.
It is not fully understood how high salt intake increases blood pressure since the RAAS system is activated when blood concentrations are low and sodium needs to be retained. This is even more complicated because not everybody is affected by a high salt intake. More than 50% of Americans are salt sensitive. This phenotype is more pronounced in Black Americans. A plausible explanation might be that salt sensitive individuals do not excrete excess sodium effectively and quickly. High sodium blood concentrations lead to fluid retention which will result in an increase of blood pressure.
Obesity Leads to a Combination of Excessive Sympathetic Activation, RAAS Overactivity, Increased Cardiac Output: Blood Pressure Increases
While genetic factors and some diseases can lead to hypertension, the major driver for hypertension today is obesity. Three mechanisms contribute to hypertension in obesity:
- Excessive sympathetic activation
- Overactive RAAS
- Increased cardiac output leading to cardiac remodeling
Excessive Sympathetic Activation
When a person develops obesity, especially visceral obesity, several physiological changes (marked red in the infographic above) can contribute to sympathetic activation:
- Growing adipose tissue increasingly converts cortisone into cortisol, the stress hormone. As a consequence, cortisol blood levels increase and stimulate the sympathetic nervous system.
- Increasing leptin and insulin blood levels stimulate the sympathetic nervous system.
- Many obese individuals develop sleep apnea and sleep apnea is also linked to sympathetic activation.
RAAS Overactivity
Aldosterone is primarily produced and secreted by the adrenal glands, but adipose tissue can secrete aldosterone and aldosterone stimulating factors such as angiotensinogen. The larger the adipose tissue is, the more aldosterone and angiotensinogen is secreted. This leads to RAAS overactivity.
The resulting sodium and fluid retention increases blood volume and blood pressure.
Cardiac Remodeling
Increased body mass in obesity means that more tissue needs to be perfused by the blood circulation. The heart increases cardiac output in order to generate more pressure. This allows for the perfusing of the additional tissue.
After a while of harder work, the heart muscle remodels to adapt to the increased work load like any other muscle. This remodeling will predominantly affect the left ventricle resulting in hypertrophy (thickening of heart muscle) and dilation (larger ventricle).
In summary, obesity cause several changes that will increase blood pressure. The next infographic summarizes how these changes can start hypertension while physiological changes due to hypertension keep aggrevating the high blood pressure.
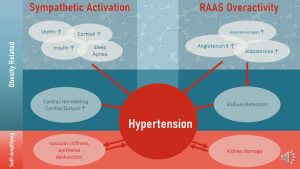
Hypertension is self-amplifying. The constant high pressure against the blood vessel walls will prompt changes in the blood vessel anatomy and damage the endothelium:
- Vascular Stiffness: Initially, the persistently high pressure against the blood vessel wall induces a thickening of the smooth muscles. This keep the blood vessel from dilating too much. The blood vessel becomes ‘buff’ and the additional muscles make the arteries stiffer. A stiff blood vessel cannot cushion normal ups and downs in blood pressure which increases the hypertension further.
- Damage to the endothelium: In addition, small damages to the blood vessel wall due to the high pressure aggravate atherosclerotic processes. The increase of plaque in the blood vessel wall will increase stiffness further and narrows the lumen of the blood vessel. As a consequence the smooth artery muscles are not able to relax the blood vessel when pressure increases and the narrower lumen increases blood pressure further.
- Damage to Kidneys: Over time, high blood pressure can permanently weaken, harden, and narrow the arteries in the kidneys. A damaged kidney further adds to hypertension.
The hypertension is now in a vicious cycle fueling its own progression.
Obesity Related Hypertension Is Difficult to Treat
Hypertension due to a genetic predisposition or aging tends to have a singular cause. This cause can be identified and a medication prescribed for example to address a low renin production or to calm down a sympathetic nervous system. These conditions can be effectively treated with medication.

However, since obesity related hypertension is complex and multi-factorial medication may not be able to completely resolve the problem. The hypertension becomes resistant. If you think back to the beginning of this chapter some of the statistics make sense. 60 to 70 % of hypertension diagnoses are due to obesity and only a quarter of people with diagnosed hypertension mange their blood pressure well.
With available medication not always being efficient, the most promising treatment seems to be an integrated diet and lifestyle treatment. This includes weight loss, dietary intervention and increasing physical activity.
Dietary Intervention: Many dietary modifications are researched and the results are mixed. The modifications are:
- Reduction of salt intake
- Increased fruit and vegetable intake (potassium, antioxidant, anti-inflammatory nutrients)
- Lipid profile modifications to prevent CVD
- Reduced added sugar intake
- Reduced alcohol intake
Some of those intervention such as a healthier lipid profile skewed to polyunsaturated fatty acids and a reduction of added sugar show no positive impact on blood pressure but might help weight loss, lowering inflammation, and the prevention of CVD.
The other interventions have a statistically significant impact on blood pressure, but the impact is small:
| Dietary Factor | Systolic BP (mm Hg) | Diastolic BP (mmHg) |
| 5 kg weight loss | -4.4 | -3.3 |
| 1.7 g less sodium/d | -4.2 | -2.0 |
| <2 alcohol units/d | -3.3 | -2.0 |
| Beet root juice | -4.4 | -1.1 |
| Flavonoid Intake | -1.0 | -0.9 |
| Integrated diet | -9.0 | -4.3 |
| Medium- to high-intensity aerobic activity | -11 | -5 |
Consider a person with a blood pressure of 145/90. In order to get this blood pressure back to normal the systolic BP would needed to be reduced by 25 mm Hg and the diastolic BP by 10 mm Hg. This makes it clear that these individual lifestyle interventions are not enough.
How about diets that combine all those interventions into one? The DASH diet is an example for such a integrated dietary approach. Blood pressure reduction is higher with an average of 9 mm Hg systolic reduction. It it becomes clear that lifestyle intervention are a good strategy to prevent moderate hypertension from progressing to severe hypertension or return elevated blood pressure, maybe hypertension stage 1 back to normal.
For severe hypertension lifestyle interventions can still reduce the damage to the blood vessels somewhat and decrease the risk for CVD.
Weight Loss: Losing 5 -10 pounds of weight is usually enough to improve metabolic health in patients with T2D, but it is often not sufficient to bring the blood pressure back into the normal range. Many obese individuals also struggle to maintain a larger weight loss that would improve hypertension.
Therefore, bariatric surgery is a recommended treatment option for resistant hypertension as the last resort if losing weight naturally fails. According to an observational study done by the University of Southern California, 75.4 % of patients who had gastric bypass surgery experienced complete resolution of high blood pressure.
Hypertension, T2D and Cardiovascular Disease Are Inter-Connected
We tend to see the three major chronic diseases T2D, hypertension and CVD as separate diseases but they are inter-connected aggravating each other.
Obesity, especially visceral obesity is the primery driver for T2D. Glucolipotoxicity in T2D damages artery walls, contributing to endothelial disfunction (more about that in the next chapter) and vascular stiffness. These changes in vascular physiology are correlated to hypertension. Uncontrolled T2D also damages kidneys increasing the blood pressure.
Obesity on it’s own increases blood pressure even if T2D is not present. Hypertension damages the lining of the arteries leading to increasing vascular stiffness. Stiffer blood vessels are not able to adapt to fluctuations in blood pressure effectively and increase the blood pressure. Hypertension also triggers anatomical and metabolic adaptions in the heart. The heart undergoes not only a thickening of the left ventricle but chronic inflammation of the heart muscle increases.
Damaged blood vessel walls due to hypertension and T2D accelerate atherosclerotic processes increasing the risk for heart attack and stroke. Thickening of the heart muscle and damage of the heart muscle due to chronic inflammation are leading over time to a reduce the effectiveness of heart muscle contractions. The consequence is heart failure.
The next chapter will look more in depth into CVD and the connection to obesity, T2D, and hypertension.
Interested In More Information?
- https://www.acc.org/latest-in-cardiology/articles/2020/04/06/08/53/racial-disparities-in-hypertension-prevalence-and-management
- Sanders TABJ. Hypertension. In: Marriott BP, Birt DF, Stallings VA, Yates AA eds. Present Knowledge in Nutrition: Volume 2: Clinical And Applied Topics in Nutrition. London, United Kingdom: Elsevier; 2020:379-391
- Byrd-Bredbenner C, Moe G, Berning J, Kelley D. Wardlaw’s Perspectives in Nutrition. New York, NY: McGraw-Hill Education; 2019: 491-543
- https://www.cdc.gov/bloodpressure/index.htm
Editors: Nicole Legler, Eric Hanzel
NUTR251 Contributors:
- Spring 2020: Jenny Holguin, Kaye Hutchison, Tina Dinh, Jacob Sautter, Caleb Licking, Gage Gauchat, Shane Rapp, Alexander Casebeer, Mariel Sprakel, Rawan AL Jabri
- Fall 2020: Miles Judson
Lining of the blood vessel


Feedback/Errata