14 Healthy Eating During Pregnancy Might Be Difficult

As we have discussed in previous chapters, there are various nutritional recommendations for pregnant women. While women may initially accept these recommendations and plan to implement them, it is common to experience barriers throughout the pregnancy—such as nausea, vomiting, constipation, cravings, and various food restrictions—that can minimize their efforts.
New cravings and/or aversions may develop; for instance, the mother might find that she is not able to stomach foods she normally enjoys, but strangely starts craving non-food items such as ice or dirt. Hormonal changes can fuel these changes in eating patterns. To protect the fetus, the mother’s diet may also be modified through utilization of proper food safety measures—or even entirely omitting certain foods from her diet—during pregnancy.
These barriers can make it difficult for mothers to eat a well-balanced diet during their pregnancy. It is important to both acknowledge these difficulties and use strategies to reduce their negative effects in order to support healthy weight gain and minimize development issues.
You Will Learn:
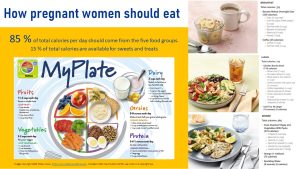
- Pregnant women should follow similar eating pattern to non-pregnant women.
- Pregnant women may experience multiple barriers to healthy eating:
- Nausea and vomiting might be triggered by raising hormone blood levels.
- Progesterone causes the gastrointestinal musculature to relax leading to an increase of acid reflux and constipation.
- Cravings and aversions are common in pregnancy, but it is unclear if these are true physiological changes with a physiological purpose.
- Pregnant women are at a higher risk for foodborne illnesses. Some can harm the fetus severely.
- Basic food safety measures are important.
- Pregnant women should not eat uncooked or undercooked meat, dairy and fish.
- Alcohol and excessive caffeine intake may cause problems during and after pregnancy.
Pregnant Women Should Follow Eating Patterns Similar to Non-Pregnant Women
We established during the last chapters that women should follow the same nutrient-dense eating pattern as non-pregnant women. This includes the healthy US eating pattern (MyPlate), the DASH diet, the Mediterranean diet, and the healthy vegetarian diet. Low-carbohydrate diets need to be adjusted by increasing carbohydrate intake. Very-low carbohydrate diets such as the Keto diet are inadequate for pregnancy.
On top of that, pregnant women should take a prenatal supplement that ensures optimal folate and iron intake. Women who do not spend sufficient time outside need a 10 µg vitamin D supplement. Iodized salt should be used when preparing foods, and vegan women must take a vitamin B12 supplement or eat sufficient amounts of vitamin B12 fortified foods.
Additional energy needs during the second (+ 340 kcal) and third trimester (+ 452 kcal) are small and should come from the same nutrient-dense foods the woman is already eating.
What about the cravings? Does that mean pregnant women cannot have any sweets and treats? The Dietary Guidelines recommend that pregnant women eat 85% of their daily energy intake as nutrient-dense, healthy, fresh foods. This leaves 15% of the daily energy intake for sweets and treats. If a woman consumes 2000 kcal in her first trimester, 300 kcal can come from the sweets and treats category. During the third trimester, this amount increases to 370 kcal. For example, a half cup of gelato is 218 kcal, fifteen potato chips are 160 kcal, and two chocolate chip cookies total 140 kcal.
Of course, these recommendations do not necessarily reflect trends in how pregnant women eat. National surveys in the US give us an idea of the actual dietary intake during pregnancy:
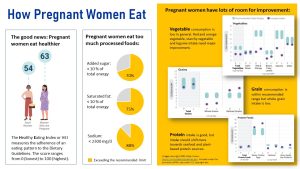
The good news is that pregnant women are eating better than non-pregnant women (left side of the infographic). What does that number mean though?
The healthy eating index or HEI compares an eating pattern against the Dietary Guidelines recommendations. The index ranges from 0 (lowest adherence) to 100 (highest adherence). When you look at the average score, the HEI goes from 54 to 63 and that tells us that there is a lot of room for improvement.
A majority of pregnant women exceed the recommended limit for added sugar, saturated fat, and sodium. These numbers indicate that most pregnant women in the US eat more processed foods than healthy, nutrient-dense foods.
Looking closer at food groups, pregnant women almost meet the fruit recommendation, but vegetable intake is too low. Look at the graphs on the right. The light blue area indicates the intake amounts we would like to see, and the purple dots show the average intake by pregnant women in the US. Women get sufficient leafy greens, but lack in red and orange vegetables. Living in an environment that vilifies carbohydrates, it is not surprising that women do not eat enough legumes (beans, peas, lentils) and starchy vegetables.
Looking at the grain intake—which is important to provide a constant flow of glucose to the fetus—we see that the grain intake is sufficient, but women need to eat more whole grains and less refined grains. This is particularly important because whole grains (and legumes from the vegetable group) provide great amounts of soluble and insoluble fiber. As you will see later in this chapter, pregnant women are prone to develop constipation. A sufficient fiber intake will ensure good gut motility.
Lastly, pregnant women get sufficient amounts of protein; however, we would like to see an increased intake of seafood because fatty fish is such a good source of omega-3 fatty acids needed for brain development of the fetus.
Pregnant Women May Experience Multiple Barriers to Healthy Eating
The recommendations are clear for pregnancy, but healthy eating is not always possible.
Pregnant women experience an initial increase of hCG and progesterone during the first trimester of the pregnancy, and then a continuous increase of estradiol and progesterone. These hormones sustain pregnancy, adapt the woman to the demands of pregnancy, and promote placenta and fetal growth—but also impact the gastrointestinal tract in various ways.
Four of the most recognizable pregnancy symptoms involved with the GI tract are nausea and vomiting, hyperemesis gravidarum, acid reflux, and constipation. In general, these conditions are not tied with negative pregnancy outcomes, but they can certainly be unpleasant for the mother and influence her food choices throughout pregnancy.
Morning Sickness Can Make Healthy Eating Difficult or Impossible
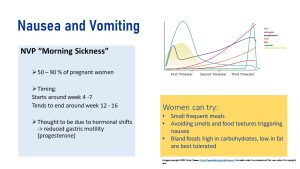
Nausea and vomiting of pregnancy (NVP) is one of the most common experiences women have in their first trimester, affecting around 70% of pregnant women. It is commonly referred to as “morning sickness,” but women may experience it at any time of the day, and the severity of symptoms varies. Symptoms tend to peak by week nine, and while NVP often improves by the start of the second semester, it can cause issues in choosing nutrient-dense foods. Women may find bland foods to be a better option, as greasy or spicy foods can aggravate the stomach. It is also important to manage fluid intake to prevent dehydration.
It is unclear which exact hormones or environmental factors contribute to NVP. One prime suspect is hCG since this early pregnancy hormone declines along with the NVP symptoms during the second trimester. Estradiol is also discussed, along with a psychological predisposition.
Despite the discomfort, NVP is associated with a stable pregnancy and positive pregnancy outcomes. This may be due to higher hormone levels that stabilize the pregnancy.
For most women, dietary and lifestyle treatment is sufficient. The first line of defense is avoiding stimuli—taste, strong smells, heat, noise—that trigger nausea. Dietary recommendations are based more on observations than solid science; small meals and avoiding spicy or fatty foods is recommended. Vitamin B6 supplements and antiemetic drugs are prescribed if the woman does not tolerate symptoms well.
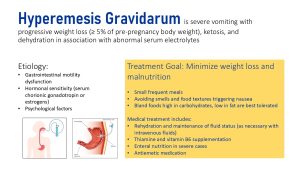
Most pregnant women experience regular NVP; however, in 0.3–2% of pregnancies, excessive vomiting known as hyperemesis gravidarum can occur. This can cause loss of hydrochloric acid from the stomach, which may lead to electrolyte imbalances of chloride, sodium, and potassium.
Women may lose weight and become dehydrated because of the excessive vomiting and inability to keep any food or fluids down. We covered that maternal weight loss should be minimized because it is an independent predictor of poor fetal outcome. However, there is currently conflicting data about hyperemesis gravidarum and its overall effect on birth weight.
Regardless of the effect on the pregnancy outcome, hyperemesis gravidarum is an extremely unpleasant experience for the mother. Similar to nausea and vomiting recommendations, it may be helpful to consume smaller, frequent meals and increase resting. Medical treatment may be necessary to correct deficiencies and hydration status.
In extreme cases of hyperemesis gravidarum it might be necessary to provide enteral nutrition using a nasogastric tube or a G-tube (see image above).
Rising Progesterone Levels Relax the Gastrointestinal Muscles, Increasing Acid Reflux and Constipation
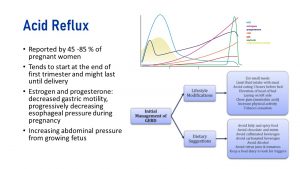
There are various factors contributing to acid reflux in pregnant women, including hormonal changes and increasing pressure (from the fetus) on the stomach. Acid reflux or “heartburn” happens when the muscles between the esophagus and stomach relax, which allows the stomach’s contents to come back up through the esophagus. This may cause a burning sensation. Acid reflux is normal and usually one of the earliest symptoms of pregnancy.
Pregnancy hormones, especially progesterone, cause the muscles in the GI tract to relax. The relaxation of muscles can cause food to move more slowly throughout the GI tract, which can result in both increased stomach acid and heartburn occurrence. While heartburn may not be pleasant for the mother, it can actually be beneficial for the baby. The slow movement of food through the GI tract allows more nutrients to be absorbed, resulting in better nutrient availability for the placenta and fetus.
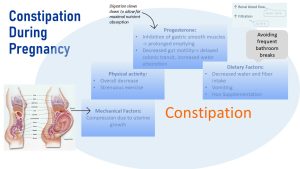
Progesterone relaxes GI muscles and reduces gut motility. This slows down digestion to allow for efficient nutrient absorption, which includes water reabsorption in the colon. This alteration contributes to constipation during pregnancy. During late pregnancy, the growing fetus and uterus press against the GI tract, further slowing down digestion.
It does not help that many American women lack fiber from fruits, vegetables, whole grains, and legumes. Fiber tends to bind water and keep stools soft. Other factors contributing to constipation include low hydration due to vomiting and iron supplements as well as decreases in physical activity during late pregnancy.
Increasing fiber consumption, fluid intake, and physical activity are recommended for smoother digestion. Fiber will help soften stool and stimulate GI motility moving the bolus forward. It is recommended to consume 25-30g of dietary fiber per day. Fiber is most abundant in fresh fruits, vegetables, whole grain breads, and legumes. Moderate exercising will also help food pass through the body by stimulating the bowels to move. It is recommended to exercise at least three times per week for 20-30 minutes.
Pregnancy Cravings and Aversions Impact Nutritional Choices
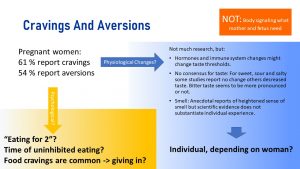
Food cravings and aversions are another often reported feature of pregnancy. 61 % of women report cravings while 54 % report aversion. Some women experience both. Scientifically, it is not clear they exist though.
One potential hypothesis suggests a change in taste threshold due to pregnancy hormones. Some pregnant women might experience bitter taste more intensely. Anecdotal evidence points toward a heightened sense of smell, which would also change taste.
When it comes to the famous cravings for sour foods the research is unclear. Some studies support changes in sweet, sour, or salty taste perception. Other studies don’t.
It is clear though that even if those changes exist, they depend very much on each individual woman. It is unclear if cravings and aversions are a physiological phenomenon or a social-cultural one.
The cultural idea of eating for 2, or a sense that pregnant women can follow cravings uninhibited, might contribute to following cravings and aversions that are normally suppressed.
Pica: During pregnancy, some women may experience pica, which is a craving for non-nutritive substances such as ice, dirt, chalk or cornstarch. There is no scientific consensus why pica develops in some pregnant women. Most explanations you read are at this point speculations. While pica may occur in pregnancy, it is not necessarily safe, as consumption of non-nutritive substances may harm the GI tract and offset intake of nutrient dense foods.
Food Safety Considerations
Food Safety Prevents Foodborne Illness for the Woman and Fetus
During pregnancy, the maternal immune system is suppressed to allow a genetically different fetus to live and grow in the woman’s body. This makes the pregnant woman more vulnerable to foodborne illnesses. Here is a review of food safety rules the family should always observe as these rules are even more important during pregnancy:
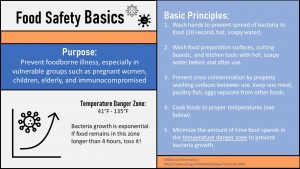
Beyond basic food safety skills, pregnant women are advised to avoid unpasteurized juice (the one in the fridge section of the grocery store) and raw sprouts. These foods carry a risk of being contaminated with bacteria from animal feces and urine. Raw meats, fish, and dairy carry the risk of four types of pathogens that are harmful to the fetus, described below.

The following pathogens cause only mild flu-like symptoms in pregnant women, but can pass through the placenta (incomplete immunological barrier) resulting in severe consequences for the fetus.
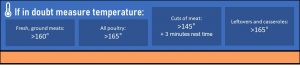
Women are advised to avoid eating undercooked meats—no medium rare steaks or burgers, or salami, for example—and avoid cleaning a cat’s litter box because of increased risk of toxoplasmosis. Toxoplasmosis is caused by the parasite toxoplasma. If a cat eats an infected mouse or raw meat, then the parasite is able to multiply inside their intestines and be excreted into their feces. Inhaling infected cat feces or cat litter can cause someone to contract the toxoplasmosis. Toxoplasmosis can cause complications such as a stillbirth, seizure, jaundice, or miscarriage.
Coxiella, commonly known as Q fever, is spread to humans from eating contaminated, undercooked meat (usually sheep, cows, and goats) and dairy products. Contact with infected feces, urine, or inhaling infected dust particles can also cause infection. Coxiella is caused by the bacterium Coxiella burnetii. If a pregnant woman becomes infected, it can cause stillbirth, miscarriage, preterm delivery, or low birth weight. This tends to be more an issue for pregnant women living on a farm or working in food production.
Foods such as raw milk, cheese from raw milk, undercooked meats, and some deli meats (salami, pepperoni) may contain Listeria monocytogenes. If consumed, a serious infection called listeriosis may occur. Listeriosis can cause miscarriage and stillbirth, as well as life-threatening infections once the infant is born.
Recently, dishes based on raw fish such as sushi, sashimi, ceviche and tartare have become popular restaurant items. Raw fish carries a risk of infection with fish-borne parasites. Since this is a recent development, for science that is, research is limited. The available research shows that parasites can infect that gastrointestinal system and might lead to anemia due to blood loss. Pregnancy anemia is connected to fetal growth restrictions and preterm delivery.
In general, pregnant women should only eat well-done meats such as burgers and steaks, and forgo raw meat deli such as salami and some hams. The milk in grocery stores is pasteurized and does not pose a risk. Raw milk is sometimes promoted as a healthier and better option in the media, but this is not true. The nutrient composition is not any different, and drinking raw milk is playing Russian roulette with the health of the fetus. Some cheeses in grocery stores, such as some swiss cheeses or gruyere, are produced from raw-milk. Reading ingredient lists will allow pregnant women to avoid these.

Aside from parasites, there is another danger associated with consuming too much of the wrong fish. Consumption of large fish should be limited during pregnancy or avoided altogether.
Methylmercury accumulates in fish through the aquatic food chain. Small fish have low levels of methylmercury but midsize fish eat lots of smaller fish accumulating the methylmercury. Ultimately the larger the fish, the more methylmercury is accumulated in the meat of the fish.
Mercury is neuro-, nephro-, and immunotoxic, and the growing fetus is especially vulnerable to the effects of mercury. Damage to the developing neurological system is likely permanent and can range from mild cognitive impairment to severe brain damage, depending on the amount of exposure.
It is a balancing act, however, because women are also recommended to increase their intake of omega-3 fatty acids during pregnancy for optimal development of the fetal nervous system and brain. Fatty fish are one of the best sources for omega-3 fatty acids with the highest bioavailability, but might also contribute methylmercury.
Since we usually see fish in neatly packaged pieces in the grocery store, which types should be avoided? Swordfish, bluefin tuna and Spanish mackerel should be avoided altogether as these fish have the highest methylmercury concentrations. Fish with moderate concentrations such as tuna, salmon, cod, and haddock should be limited to 8-12 ounces per week. Smaller fish, such as sardines, are at the bottom of the food chain and contain less methylmercury.
To summarize, it is best for women to choose fish with a lower mercury content such as sardines, salmon, or cod. The Dietary Guidelines recommend between 8 and 12 ounces per week.
Depending on geographical location and their budget, pregnant women may not have easy access to wild-caught salmon twice a week. If women have limited access to fresh fish or are concerned about methylmercury exposure, there are other sources of omega-3s such seaweed, flaxseed, chia seeds, and walnuts. Before taking a fishoil supplement the women should talk about dose and type of supplement with her gynecologist.
Alcohol and Excessive Caffeine Intake May Cause Problems During and After Pregnancy
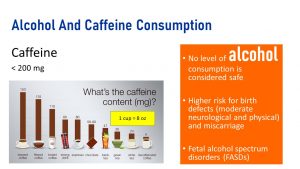
Let’s start with alcohol because the research is very clear. Women should avoid alcohol while trying to become pregnant and during pregnancy. There is no safe time during pregnancy for alcohol consumption. All types of alcohol are equally harmful.
Alcohol consumption during pregnancy can cause miscarriage, stillbirth, and a range of lifelong physical, behavioral, and intellectual disabilities. Drinking alcohol during the first weeks (when organs and tissues develop) can lead to changes in facial features.
The vulnerable, developing neurological system can be impacted in varying degrees—at any time during the pregnancy—and can lead to long-term memory, attention and behavior problems in the child. These disabilities are known as fetal alcohol spectrum disorders (FASDs).
On the other hand, caffeine research is not as clear. Naturally, scientists cannot research the effects of caffeine on the human fetus. This would be unethical. The existing research was conducted in mice and results from studies asking mothers about their caffeine consumption, retrospectively, after pregnancy.
After consumption, caffeine crosses the placenta and can be found in the umbilical cord blood, fetal blood, and amniotic fluid. In animal studies, caffeine seems to reduce the blood flow to the placenta. Based on this research, scientists are concerned about low birth weight newborns and an increased risk for miscarriage when caffeine intake is high.
The scientific evidence is at this point is inconclusive but it seems to be clear that moderate caffeine consumption is not a concern. Pregnant women should limit the amount of caffeine to less than 200 mg per day.
How much in terms of caffeinated drinks is 200 mg? It depends what beverage consumed. A brewed coffee house coffee has around 150 mg of caffeine. One cup—small 8 ounce not a big 12 ounce mug—would be enough. One can of energy drink can have 111 mg of caffeine per 12 ounce can. A mug of black tea would be around 75 mg.
Interested in More Information?
Alcohol Use in Pregnancy (CDC): https://www.cdc.gov/ncbddd/fasd/alcohol-use.html
Editor: Meryn Potts, Gabi Ziegler
NUTR251 Contributors:
- Spring 2020: Haley Jensen, Hailie Slepicka, Alonda Iturbide, Brittany Southall, Eugene Baraka
- Fall 2020: Shalin Bhakta


Feedback/Errata
18 Responses to Healthy Eating During Pregnancy Might Be Difficult