12 Nutrient Transfer During Pregnancy
Sabine Zempleni

By week 10-12, the placenta has matured enough to connect the tiny fetus to the mother’s blood vessel system. The lacuna space between maternal and fetal side of the placenta can be filled with blood, and hemotrophic nutrition to the fetus can begin. During the second and third trimester, the placenta keeps maturing and growing to adapt to the increasing nutrient needs of the fetus. That way, the tiny 0.5-ounce fetus from week 12 can grow into a 7.5-pound newborn. Our focus shifts now from maternal adaptations to the fetus.
You Will Learn:
- The placenta mediates between fetus and mother.
- The placenta has similar nutrient transport mechanisms than the small intestine.
- Some nutrients are transported along a concentration gradient
- Some nutrients can be accumulated in the fetus even if the mother has a low intake
- Nutrient needs start increasing during the second trimester, reaching a peak during the weeks before birth.
- Glucose is the main energy source for the fetus.
- Maternal metabolic conservation measures provide the additional protein for fetal growth.
- Fat is a building block for the fetus and not an energy source.
- Selected micronutrients need special attention: Iron, iodine, vitamin D and folate.
- Does a mother need to eat for two?
Nutrient Needs Start Increasing During the Second Trimester Reaching a Peak During the Weeks Before Birth
During the first weeks of pregnancy the fetus will require very little nutrients and histiotrophic nutrition will suffice. When does the mother need to eat for two, or is this ever necessary?

After all organs are mapped out, the fetal growth starts to accelerate after 16 weeks. Interestingly the growing fetus does not only gain weight—See the bend in the curve around week 24 in the lower left graph above when growth speeds up?—but the body composition changes as well.
An adult human has a water content of 50-60%. A fetus at 25 weeks of gestation is mostly water—88%—and has very little body fat, only 1%. Throughout the remaining pregnancy, the body water comes down to 75%, fat free mass increases, and during the last weeks of pregnancy the fetus accumulates fat deposits.
Along with fat deposits, the fetus will now accumulate fat soluble vitamin stores, as well as stores for some minerals.
The important part is that the need for some nutrients and energy increases during the second trimester. Other nutrients such as fat-soluble vitamins do not have an increased need until the final weeks of the pregnancy.
I know, I have not answered the Eating for Two question. I will get to it. First, we will have a look how the nutrients get to the fetus.
The Placenta Mediates Between Fetus and Mother

Maternal and fetal blood vessel systems are closely located next to each other, but are not directly connected. The placenta separates and mediates between mother and fetus.
The placenta is a spongy, pancake shaped organ with a weight proportional to the fetus. If the fetus is small, the placenta will be small, and vice versa. If the placenta cannot form and grow optimally, the fetus will experience intrauterine growth restriction which can lead to the loss of the fetus, premature delivery or SGA newborns. The placenta is embedded into the maternal endometrium and grown from the outer layers of the blastocyst, the trophoblast. The umbilical cord, grown from the embryoblast, connects the placenta to the fetus.
The placenta has multiple functions that can be summarized as (1) transport and metabolism, (2) endocrine organ, and (3) protection of the fetus.
The first function is obvious. The placenta shuttles oxygen, water, and nutrients from the maternal blood circulation to the fetal blood circulation. On the opposite route, the placenta shuttles waste and CO2 to the maternal blood circulation for excretion. What is less obvious is that the placenta also synthesizes glycogen, cholesterol, and fatty acids. These nutrients can be used by the placenta or transported to the fetus.
You already learned about the second function, synthesizing and secreting hormones. The main hormones produced are progesterone, estradiol, and hCG, as well as other hormones and bioactive compounds that orchestrate growth and development in the fetus and adaptations in the mother. Here is an interesting fact: the placenta does not have any nerves, so the only communication method between mother, fetus, and placenta is by hormone secretion and bioactive proteins.
Lastly, the placenta protects the fetus, though not completely. The membranes between maternal and fetal side can filter out larger molecules such as potentially toxic substances, viruses, and bacteria. The barrier function is imperfect as some viruses, bacteria, and smaller potentially toxic molecules can pass through.
The placenta also secretes antivirals and activates the maternal immune system against bacterial infection to protect the fetus. This does not mean that the placenta is sealing the fetus off perfectly—some viral diseases, for example, the zika virus can be transferred.
Around week 16, the placenta starts transporting immune globulins from the mother to the fetus. This transfer increases at the end of the pregnancy. At term, the fetus has a greater serum concentration of maternally derived IgG than does the mother. The IgG acts like an early vaccination protecting against diseases the mother is exposed to.
The next question is how the placenta transfers nutrients to the fetus and removes waste. First, we will look at the general concept, then focus in on the details.

Anatomically, the placenta has three parts. On the right side of the graphic, you see the maternal side called basal plate. On the left is the fetal side, the chorionic plate. Between the basal and chorionic plates is a large cavern called the intervillous space (IVS) or lacuna. As you see maternal and fetal circulation are extremely close but still separated by cell layers.
How does the transfer of nutrients, oxygen, and carbon dioxide work?
On the maternal side, you can see corkscrew shaped blood vessels. These maternal spiral arteries have a high pressure and squirt oxygen- and nutrient-rich arterial blood into the intervillous space. You can imagine this like a hot tub; the intervillous space is the tub and the jets squirt blood into it.
On the fetal side, branched villi reach into this tub of blood and are anchored to the basal plate. Those villi are lined with an absorptive layer of merged cells containing multiple nuclei, called the syncytiotrophoblast (I know, looks unpronounceable).
After nutrients and oxygen are absorbed, they leave the syncytiotrophoblast on the opposite side into blood vessels located in the center of the villi. The blood vessels inside the villi are collected into the umbilical cord consisting of one vein and two arteries twisted around each other.
Here is an interesting terminology difference:
In the mother, arteries carry oxygen rich blood and nutrients away from the heart, while veins carry CO2 and waste toward the heart.
The same definition applies to the umbilical cord:
- The umbilical vein leads away from the placenta toward the heart of the fetus, and carries oxygen and nutrients from the mother (not CO2 and waste as we would expect).
- The two umbilical arteries carry CO2 and waste away from the heart of the fetus toward the placenta.
Think about that for a minute, this terminology can be confusing!
On the fetal side, the villi absorb nutrients and oxygen from the intervillous space and release CO2 and waste products into the intervillous space. The maternal side releases oxygen and nutrients into the intervillous space and takes up the CO2 and waste products into the maternal blood circulation carrying it away to the lung, liver, and kidney for removal.
The Placenta Has Nutrient Transport Mechanisms Similar to the Small Intestine
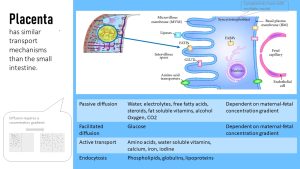
The transport mechanisms for nutrients on the fetal side of the placenta are very similar to what you learned about the absorptive mechanisms in the small intestine.
Those mechanisms are:
- Passive diffusion
- Facilitated diffusion
- Active transport
- Endocytosis
Some Nutrients Are Transported Along a Concentration Gradient
Water, electrolytes, free fatty acids, steroids, fat soluble vitamins, alcohol, oxygen, and CO2 can diffuse from the IVS through the epithelial cells on the fetal side to be released into the fetal vein. Remember that diffusion can only work if the concentration of the solute on the maternal side is higher than the concentration on the fetal side.
Other cells still need the concentration gradient, but they are transported by transporter-facilitated diffusion. Glucose is transported that way. For glucose, the common insulin dependent GLUT transporter is integrated into the epithelium enabling facilitated diffusion of glucose into the syncytiotrophoblast. On the fetal side there is another GLUT transporter shuttling glucose into the fetal capillary.
Nutrients transported by diffusion and facilitated diffusion require a concentration gradient to reach the fetus. For example, the mother’s blood glucose needs to be high enough so blood in the IVS has a higher glucose concentration than the fetal circulation. This is where the physiological insulin resistance comes in. This adaptation will ensure that the maternal blood glucose concentrations are elevated longer after a meal.
Some Nutrients Can Be Accumulated in the Fetus Even if the Mother Has a Low Intake
Amino acids, water, soluble vitamins, calcium, iron, and iodine require an ATP dependent transporter. This means that even if the maternal blood concentrations are not high, the placenta can filter out those nutrients and accumulate them on the fetal side (to a certain degree). For example, iron deficiency anemia will still have a negative impact on the fetus.
Phospholipids, lipoproteins, and immunoglobulins are taken up by the villi via endocytosis. VLDL and LDL bind to their respective receptors. The receptor mediates endocytosis, the engulfing of the large molecule by the cell wall.
Glucose Is the Main Energy Source for the Fetus
The main energy-yielding nutrients for the fetus are glucose, and to a lesser degree amino acids. The fetus is not able to use fat as an energy source. Long chain fatty acids are needed, but as building blocks for growing tissues only.
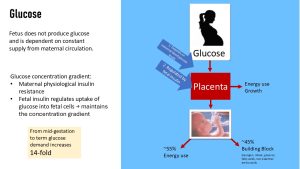
The fetus does not produce glucose via gluconeogenesis. Since glucose is the main energy source for the fetus, and is also used as a building block, a constant flow of glucose from the mother is necessary to support optimal fetal growth.
From mid-gestation to term, the glucose demand increases 14-fold. To meet this demand, the mother’s insulin sensitivity will decline somewhat (=physiological insulin resistance). Insulin dependent maternal tissues such as muscles and liver will take up less glucose. That way maternal glucose blood concentrations remain elevated longer after a meal. This is the same mechanism you learned about in the T2D chapter.
This metabolic adaptation allows for a higher glucose concentration in the IVS in the placenta.
GLUT1 and GLUT4 are insulin independent glucose transporter. When fetal blood glucose levels are rising, fetal insulin is secreted allowing for glucose transport into the cells. This maintains the concentration gradient between fetal blood and intervillous space.
Once the glucose is circulating in the fetal cardiovascular system, about 55% is directed to cells for energy use and 45% is used as building blocks for non-essential amino acids, ribose (DNA), and glycerol (triglycerides).
Maternal Metabolic Conservation Measures Provide the Additional Protein for Fetal Growth
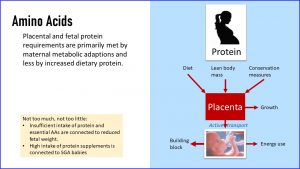
Since the fetus and placenta are growing rapidly during the second half of the pregnancy, one would think that the mother should increase her protein intake substantially. This is not correct.
Most of the additional need for fetal and placental growth is covered by maternal metabolic adaptations. Amino acids that are transferred to the fetus stem from the maternal diet, conservation measures, and if protein intake is low from the mother’s lean body mass.
Again, the placenta diverts some of the amino acids for its own growth and maintenance. The remainder is actively transported to the fetus. Interesting fact: The fetus has higher amino acid blood concentrations than the mother, which can only be achieved using an active transport mechanism. Most of those amino acids are used for tissue synthesis and if glucose is in short supply for energy purposes.
In today’s society, more protein is often considered better, and many Americans tend to over consume protein. Protein shakes are part of many people’s daily routine. A pregnant woman needs to rethink here. While insufficient protein intake, especially when essential amino acids are missing, is connected to reduced fetal growth, high protein intake is connected to slowed fetal growth as well. Studies show that a high intake of protein supplements is connected to newborns that are small for their gestational age. Why? Not clear yet.
Fat Is a Building Block for the Fetus and Not an Energy Source
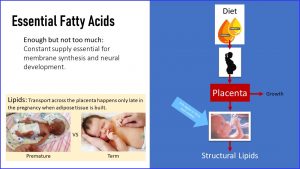
During the pregnancy, fat is not an energy source for the fetus. Unsaturated long chain fatty acids are transferred to the fetus and are needed as building blocks for cell membranes and brain.
Sufficient essential (omega-3 and omega-6) fatty acids translate into higher birthweight and larger head circumferences. Low supply of essential fatty acids is connected to lower cognitive capabilities. On the other hand, too many essential fatty acids increase peroxidation, and therefore will require more antioxidants to avoid oxidative damage to fetal cells.
Many American women have an imbalanced intake of essential fatty acids: too much omega-6 fatty acids (from soybean, corn, sunflower or safflower oils, and meat) and insufficient amounts of omega-3 fatty acids (fatty fish, walnuts, and some seeds). At this point, it is unclear if American women who have a low omega-3 intake would benefit from fish oil supplementation during pregnancy. Omega-3 fatty acid supplementation in the form of DHA is also discussed in preventing preterm birth.
Increased transfer of fatty acids takes place during the last weeks of pregnancy. This fat is not used as an energy source, but to build fetal adipose tissue.
Selected Micronutrients Need Special Attention: Iron, Iodine, Vitamin D and Folate
Most mothers in the US have a reasonable micronutrient intake to provide the fetus with sufficient amounts. Mineral deficiencies are more likely in vegetarian and vegans (Fe and Zn), as well as low-income populations and people living in poverty. A few minerals and vitamins need to be highlighted because intake in the US is not always optimal.
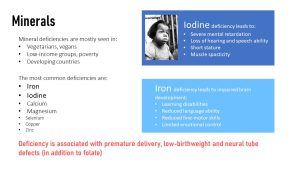
The first mineral is iron. You already learned in the pre-conception section that iron deficiency should be addressed before pregnancy because iron stores take time to recover.
Severe iron deficiency in pregnancy impacts the development of the brain and nervous system. The long-term consequences are learning disabilities, reduced language ability, reduced fine-motor skills, and limited emotional control.
Scientists also suspect that a low maternal iron status without full anemia might be connected to a mild version of the consequences of inadequate iron supply. Here is the problem. It is difficult to link mild cognitive impairment and lower emotional control directly to iron deficiency because many other factors can play a role as well.
Iodine was a problem nutrient during pregnancy in the past, and is still a problem in developing countries. Before the introduction of iodine, landlocked areas of the US such as the Great Lakes, Appalachians, and Northwestern regions had a high prevalence of iodine deficiency. This was because the soil of these areas did not contain much iodine, and thus the food produced did not provide much iodine either. These areas were called the goiter belt because many people had visibly enlarged thyroids, called a goiter, due to iodine deficiency. Starting in 1924, iodized salt became available for purchase; today, iodine deficiency is rare in the USA.
If a mother is iodine deficient, the lack of iodine will lead to a goiter in the mother, but severe brain damage in the infant. Optimal neurological development of the fetus requires sufficient amounts of both iron and iodine. Iodine deficiency during pregnancy leads to intellectul disability, loss of hearing and speech ability, short stature, and muscle spasticity.
If the mother has a suboptimal calcium intake, the fetus will not experience negative effects. When calcium blood levels fall below a threshold, maternal calcium in the bone reservoir will be activated and calcium absorption rate in the small intestine is increased. The negative impact will be experienced by the mother as she loses bone mass during pregnancy, increasing the risk for developing osteoporosis later in life. Therefore, it is important that pregnant women have an adequate calcium intake.
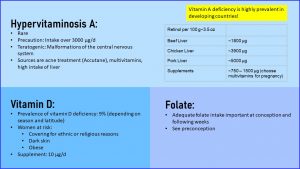
The main vitamins we need to look at are folate and vitamin D.
As you already know, adequate folate intake is essential for the development of the spinal column. Inadequate folate intake increases the risk for spina bifida and anencephaly. An infant with spina bifida might have a severe physical disability, while a fetus with anencephaly will not survive.
Vitamin D deficiency or suboptimal status does not affect all women. Low vitamin D status is more pronounced in winter for all women, especially in Northern latitudes. Other groups at risk are women who cover their skin for religious reasons, have a dark skin, or are obese.
Americans have a sufficient intake of vitamin A, but high intake of vitamin A—not carotenoids—during the pregnancy is teratogenic and will lead to issues with neurological development of the fetus. Sources of high vitamin A intake are Accutane treatment for acne, multivitamins (prenatal vitamins only contain carotenoids, no retinoids), and liver consumption.
Most Americans do not eat liver on a regular basis. If health care professionals work with ethnic minorities, this needs to be kept in mind since many cultures see liver as a healthy, nutrient-rich food.
Liver is the storage site for vitamin A, and naturally contains a high amount of it. In addition, animal feed is often enriched with vitamin A, leading to the high concentrations you see in the graphic above for pork and chicken liver.
Finally, Does a Mother Need to Eat for Two?
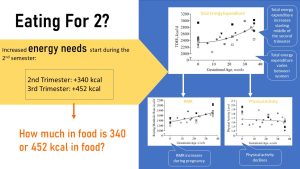
So far you learned that during the first trimester and part of the second trimester, the focus is much more on mapping out and developing organs. This process requires very little additional energy and nutrients, so the pregnant woman should eat normal amounts of food. Additional energy and nutrients (with the exception of folate) are not recommended for the first trimester.
During the second semester, the fetus and the placenta start growing rapidly. The question is now how much energy and nutrients does this growth require?
Looking at the graphs above, you will see in the top graph that the total energy expenditure increases starting in the middle of the second trimester. You also see that the additional need for energy varies a lot from woman to woman (each dot represents a woman).
Energy expenditure has several components: the RMR, thermic effect of food, physical activity, and adaptive thermogenesis. The component that increases during pregnancy is the RMR (seen on the lower left), which includes the extra energy for pregnancy and physical activity.
By the end of the pregnancy, the RMR increases 10-20%. At the same time, the physical activity portion declines for most women, which cancels out some of the increase in RMR. Since physical activity varies widely in pregnant women, the total energy expenditure will too.
Overall, the extra need for energy is small. No mother needs to eat for two.
The energy recommendations are based on the additional tissue accretion—fetus and placenta—during pregnancy. During the second trimester, an energy increase of 340 kcal per day is recommended, while during the third trimester this recommendation increases to 452 kcal per day. If you think in terms of food, this is not even an entire meal, more a substantial snack.
The second question is whether pregnant women have a disproportionately high need for micronutrients.
If you look at the two graphs below, you will see that only a few micronutrients need special attention. Recommended additional nutrient requirements for the third trimester are given by percent; the blue line shows recommended energy intake. The 452 kcal would be roughly a 23% increase if the woman ate 2000 kcal before pregnancy.
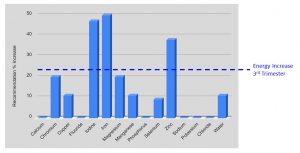
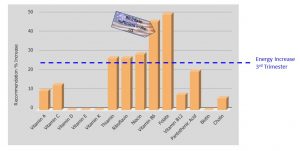
If we assume that the woman eats a healthy diet and adds some healthy foods worth 452 kcal, then most nutrients would be covered by eating slightly more food. The additional nutrient requirement is not disproportional for most nutrients, with the exception of iodine, iron, zinc, vitamins B6, and folate.
American women have more than sufficient vitamin B6 intake, predominantly from protein foods, that covers this additional need easily. Folate, as you already learned, should be supplemented. Iodine can be supplied by iodized salt intake. The only true problem nutrient is iron. In the US, pregnant women are prescribed prenatal vitamins that contain iron and folate.
With knowledge about fetal nutrient needs, you will easily understand the nutrition recommendations for pregnancy. You will also be able to see why some popular eating patterns, such as the keto diet, are less than ideal for pregnant women.
Editor: Gabi Ziegler
NUTR251 Contributors:
- Spring 2020: Eugene Baraka, Dario Henry, Eli Havekost, Kenyon Gaar
- Fall 2020: Morgan McCain, Carly Schwager, Felicity Bowers
The exchange of nutritients between the maternal and fetal blood circulations
Nutrients and extracellular material derived from the endometrial glands and blood vessels accumulates in the lacunae and is transported via phagocytosis into the yolk sac. The yolk sac feeds the embryo during the first trimester.
Immunoglobulin G is the main antibody found in blood and extracellular fluid. The function is to control infection of body tissues.
Metabolic pathway forming glucose from precursors such as glycerol, lactate, pyruvate, and glucogenic amino acids
Basal metabolic rate; RMR (resting metabolic rate) and BMR are often used interchangeably. The RMR is slightly higher than the BMR because the RMR does not require a fasted state. measure and slightly higher than the BMR


Feedback/Errata
20 Responses to Nutrient Transfer During Pregnancy