19 Transitioning to Solids And Family Meals
Sabine Zempleni
The infant is growing and developing rapidly. She learns to roll from her back to her tummy, grabs at everything she can reach, shows interest when parents are eating, and “helps” to feed herself by putting her hand on the bottle during meal time. Seeing this rapid development of their infants and seeing the range of cutely packaged interesting baby foods and meals at the grocery store, parents often can’t wait to see how the baby eats other foods rather than just milk. The cuteness overload of TikTok videos showing infants making hilarious faces trying new foods makes it even harder to wait.
It is not surprising that the majority of American parents don’t wait for the recommended 4 to 6 months to start feeding solids. At this point in this course you should have a good understanding why nutritionists and pediatricians are not just overly protective when they try to get parents to the 6-months mark.
Once the infant hits the 6 months mark health professionals change their tune completely. The parent on the other hand will learn quickly that the calm bottle feeding times can morph into messy, sometimes frustrating parts of the day—meal time. No matter how picky the little eater, how messy meal times become, the infant must have now solids in addition to milk.
The infographic below shows some developmental highlights on the left and the feeding development on the right. Note that some developmental stages and feeding correspond.

You Will Learn:
- At 6 month complimentary foods become necessary to supplement breastmilk or formula.
- Breastmilk does not provide enough energy and iron during the second 6 months of life
- Kidneys and GI tract have matured enough to handle solid foods
- Incoming teeth make reducing disaccharides necessary
- The psychosocial role of food becomes increasingly important
- How Do Parents Tell If the Infant is Ready For Solids?
- Which Foods and When to Introduce?
- The baby food becomes gradually more solid
- New foods need to be introduced one at a time
- At 8 months baby meals start to resemble healthy MyPlate meals
- Responsive feeding: Parents need to become familiar with their child’s eating cues
- Excursion: Different cultures have different approaches to introducing foods
- Many American parents do not follow the recommendations
- Healthy eating or feeding mistakes?
- The vegetarian baby
- Vegan mothers and babies
- Baby bottle tooth decay
- Allergy recommendations have profoundly changed during the last years
At 6 Month Complimentary Foods Become Necessary to Supplement Breastmilk or Formula
Don’t imagine the 6 month mark as a hard line that should not be overstepped. Think about it as around the 6 month mark. Some infants growing in higher percentiles might need additional nutrients before that point. The production of human milk can also vary between women and the amount increases only minimally at this point. Tracking the baby’s growth on the growth chart is important so the pediatrician can identify if the weight starts dropping from the infant’s growth percentile.
The lack of sufficient energy from breast milk is the most obvious reason to start feeding solids—the parents could just start adding formula—there are several other reasons that make solid feeding now necessary.
Breastmilk Does Not Provide Sufficient Energy and Iron Anymore
During the first four to six months of life breastmilk is sufficient to provide energy and nutrients for growth and development of most infants. As we discussed, breastmilk supply increases only slowly after the first month, and after six months the milk amount is not sufficient anymore to provide the increasingly active infant with enough energy for optimal growth.
Infants who are nursed without solids tend to drop off their growth percentile, first for weight, and if the situation is not fixed, the length drop-off will follow.
In addition, breastmilk is low in iron. This is not a problem during the first 6 months because during the last weeks of pregnancy iron stores are build in the fetus. Those iron stores tend to be depleted around the end of the 6th month and other nutritional iron sources become necessary.
Formula has sufficient amounts of iron but the liquid nature of the formula does not provide the energy density to satisfy the increasing energy needs of the active infant. The infant would need to drink lots of formula, and infant stomachs are small. While solids are now introduced and the amount is steadily increasing, the American Academy of Pediatrics still recommends to keep feeding human milk, nursing or pumped, until the end of the first year. If mothers decide to stop breastfeeding or pumping milk the infant still needs formula meals until the end of the first year.
Kidneys and GI Tract Have Matured Enough to Handle Solid Foods
Kidneys reach the capacity to concentrate or dilute urine as needed around the end of the 4th month. This means that the food does not need to have a low and consistent PRSL anymore. Other infant appropriate foods and additional water could be fed. This doesn’t mean that the baby can now eat salty foods like fries, burgers and chicken nuggets. Baby food should still be unsalted during the first year.
The digestive capacity of the GI system is now near adult capacity, and this allows for the digestion of a variety of foods starting around the 6 months mark.
Incoming Teeth Make Reducing Disaccharides Necessary
The lower central incisors are the first teeth to come in. The normal timing is between 6 and 10 months but some infants have teeth erupting before that time. Those baby teeth are sensitive to being flushed with sugary liquids which increases the risk for tooth decay.
Once the infant has teeth—of course they need to be wiped with a damp cloth after a meal—sugar (lactose and sucrose) in the diet needs to be reduced. As you know, breastmilk has high amounts of lactose and formula has either lactose or sucrose. Both need to be step-by-step replaced with vegetables, fruits, cereals and strained meats. Most infants are able to practice drinking from a sippy cup at 6 months. The parents should therefore think about shifting slowly away from the bottle because bottle feeding surrounds the teeth with a sugary liquid for a prolonged time. By 12 months the infant should fully graduate from the bottle to a sippy cup. Letting a teething baby fall asleep suckling at a bottle can lead to horrible tooth decay (see below.)
The Psychosocial Role of Food Becomes Increasingly Important
Around the age of six months the infant becomes interested in eating what the family eats. For humans, eating is not just curbing hunger, but a social event. We like to share food, eat in company, explore foods, and enjoy good conversation at the dinner table. The infant is ready to start the transition from being fed to eating. This transition includes the baby version of the foods the family eats—more details later in this chapter—, sitting upright in a highchair while being fed, and practicing motor skills that ultimately allow the child to feed themselves. From there, the infant will transition all the way to the family table.
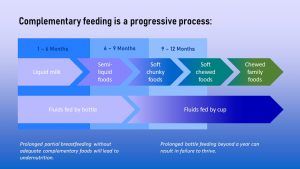
The chart below summarizes this transition from being fed milk exclusively to eating at the family dinner table:
Which Foods and When to Introduce?
Those TikToks of babies trying lemons or vegetables are entertaining to watch. Real life solid feeding and transitioning to family meals is more complicated. The shelves of grocery stores offer a huge variety of options and tend to be overwhelming for new inexperienced parents.
How Do Parents Tell If the Infant is Ready For Solids?
Per recommendations parents should stay away from solids until the end of the 4th month. At the end of the fifth month all babies should be ready for spoon feeding. This leaves us with a span of a month to start feeding solids. There are a bunch of other cues parents should watch out to see if their infant is ready:
- Holding the head up for longer periods
- Being able to sit in a high chair
- Opening/closing mouth for a spoon
- Keeping tongue flat when spoon is in mouth (tongue thrust and gag reflex have waned)
- Being able to signal when hungry or full
- Showing an interest in food
“Helping” when drinking from a bottle, trying to reach for food or needing a middle-of-the-night bottle are not cues that indicate that infant need to start solids.
The Baby Food Becomes Gradually More Solid
First, a disclaimer, solids are far from solid foods but have initially the consistency of watery apple sauce.
The baby shows the signs that she is ready for solids and is between 5 and 6 months old. What now?
The first step in the process to the family table is semi-liquid, strained foods. The first solid food is more a practice food and depends on the parents’ food culture. In any case the first foods the parents introduce should be thin and strained. Some infants will catch on fast, other will require more parental patience until they get used to the new falvor and texture.
Since the gag reflex is gone the infant is now prone to choking on food pieces. Foods that could be a choking hazard such as hot dogs, popcorn, or whole grapes—they are the perfect size to get stuck in the trachea—must not be fed until the child is much older.
Once eating from a spoon is mastered, the thin strained food can become a thicker puree version. Soft-chewed or mashed foods can be introduced When the infant is 8 to 9 months old. After the child has practiced eating the mashed foods, the next step would be foods that need some chewing, such as soft chopped or ground foods.
At the same time infants transition from being fed with a spoon to feeding themselves (still no hotdog pieces, grapes and other choking hazard foods.)
Along with progressing feeding skills, jaw muscles and chewing coordination develop as infants eat increasingly solid foods at the recommended ages. This development does not only improve eating skills but is essential for speech development later on.
New Foods Need to be Introduced One at a Time Until Meals Form
After matching the food consistency to the development of the infant, the next big question is, what foods to choose and in what order. The answer to this question depends on the food culture of the parents. First, lets have a look at the common practice in the US that informs recommendations.
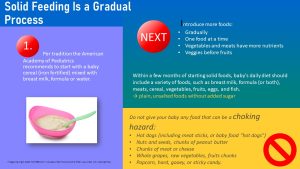
It is recommended to introduce “single-ingredient” foods one at a time with a week in between each new food. The reason for this recommendation is that some infants develop allergies and we want to make sure that parents can clearly identify if a food is not tolerated. An example of a meal that could be introduced is iron-fortified baby cereal mixed with breast milk, formula, or water. The parents already know that the infant tolerates breastmilk or formula and the new food tested is the cereal.
Since vegetables and meats have more nutrients than fruits, it is recommended to introduce those first. Sweet fruits should be introduced after vegetables so the infant does not refuse the bitter tasting vegetables once they realize that there is something better and sweeter. Within a few months of eating solid foods, the baby’s diet should consist of a variety of foods such as milk, eggs, fish, meats, veggies, and fruits. Keep in mind that the infant is not a foodie in need for different, exciting flavors at every meal. A good rotation of local, cultural appropriate foods is sufficient.

As more and more foods are introduced, meals mimicking the adult food culture start forming. Above is a sample menu for an 8-12 month old baby. Notice that the meals are baby versions of healthy MyPlate meals. Parents should choose plain vegetables, fruits, meats and cereals. Those foods can be home prepared from unsalted, unsweetened ingredients or bought as dedicated baby foods. In any case, parents should read labels and avoid added sugar.
Responsive Feeding: Parents Need to Become Familiar With Their Child’s Eating Cues
While the infant learns to master a spoon and to tolerate strange flavors (aka veggies) the parents need to learn as well. Parents should never force the infant to eat. Since the baby is not talking they need to observe the infant and learn how to read the non-verbal cues. For example, turning the head away after eating a portion of the meal indicates that the baby is full.
This doesn’t mean that an infant rejecting a new veggie should never try that veggie again. Patiently offering the rejected foods several times will do the trick in most infants. You will learn more about the taste world of infants in the next chapter.
One word about fruit juice: Fruit juice is a popular drink to introduce because infants love how sweet it is and parents think of it as healthy. However, most fruit juices, even 100 % fruit juice, contain lots of sugar. Parents should keep in mind that they are generating habits. The baby will drink water or water flavored with a little fruit juice unless parents get the baby hooked on the sweet juice. Avoiding fruit juice as long as possible will help to move the baby away from all-sweet food (more about that later in the taste chapter).
Excursion: Different Cultures Have Different Approaches to Introducing Foods
Health care providers often make the mistake applying the US recommendations to everybody. But, different cultures have different traditions when it comes to starting solids and transitioning baby to family meals.
Every culture has a first food and some cultures make this important step in baby’s life a family celebration. For example, while US parents tend to start off with cereal, most German parents start with strained carrots. In Japan, many parents integrate rice, fish and pickled vegetables into baby foods.
Below is a chart that shows some commonly used introductory baby foods in various countries.
| Country/ Region | Most common Baby First Foods? |
| China | rice porridge, mashed fruits, soft veggies, tofu, and fish |
| Japan | Rice cereal and radishes |
| India | Daliya (cracked wheat), followed by Khichdi (mushy rice-and-lentil-based dish) |
| Middle East | Hummus and baba ganoush |
| Mexico | Soft tortillas, rice |
| South Africa | Corn porridge and fish |
| Thailand | Khao tom (rice soup) |
| Germany | Pureed potatoes and vegetables |
| United Kingdom | Rice cereal, pureed vegetables, fruit |
| United States | Pureed sweet potatoes, peas |
Even recommendations for feeding baby during the first year can be different. Below is the official recommendation from Germany:
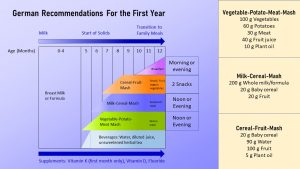
In Germany parents start with strained carrots as a spoon-feeding practice food. The veggie transitions into a vegetable-potato-meat-puree meal which replaces a milk meal between 5 and 6 months. This meal is full of iron and zinc and therefore provides exactly what breastmilk lacks. Drinks such as unsweetened herbal tea, water, and diluted juice are also introduced. At 6-7 months, a milk-grain mash is served for dinner replacing another milk meal. Whole milk, formula, or breast milk are all acceptable to use. The last mash that should be introduced between 7 and 8 months consists of fruit and cereal. Fruit helps the body absorb the iron contained in the grains.
Many American Parents Do Not Follow Recommendations

Let’s summarize the reasons why nutrition professionals recommend to wait until at least the end of the 4th month, ideally 6 months, to introduce solids:
- Human milk and formula deliver all nutrients needed for growth and development until 4 to 6 months.
- The infant has still strong reflexes that prevent efficient feeding with a spoon before the age of 4 months.
- The kidneys, digestion, gut microbiome, and immune system need time to develop fully and optimally.
In addition, long-term research indicates that babies who start solid foods before the end of the 4th month are at a higher risk for obesity and chronic diseases later in life.
The infographic above summarizes the results of a study investigating what parents feed during the first year and why they start feeding solids early (the scientists asked mothers but of course parents make those decisions.)
17 % of the mothers fed solids before the end of the 4th month. The top food was baby cereal. You can also see that mothers feeding formula are much more likely to feed solids early. When asked why they feed solids that early, mothers stated that it’s more fun at meal times, the baby is less fussy and sleeps better at night, and they have concerns that their baby is not growing well enough.
In general, mothers who feed solids early are less aware of the infant’s hunger and satiety cues. This might be part of the explanation why early solid feeding is linked to higher obesity risk.
Health Eating or Feeding Mistakes?
The Vegetarian Baby

When parents follow a vegetarian lifestyle, they often don’t think twice about omitting meat from the baby’s diet as well. Make sure to differentiate between vegetarian and vegan. We will get to vegan next.
A vegetarian eating pattern can provide all the nutrients the the growing baby needs but it might be more difficult. Parents feeding their baby a vegetarian diet should be well educated how to avoid common nutrient shortages.
Theoretically, vegetarian babies might not get enough iron due to the non-hem iron they are relying on. Sufficient iron intake is essential for the optimal development of the nervous system and brain. Choosing iron-fortified cereal and combining iron-rich cerals and vegetables with vitamin C-rich fruits will help.
A sufficient protein intake should not be a problem if the infant consumes enough milk, eggs, and a mix of plant protein.
Breastmilk and formula delivers sufficient calcium, but vitamin D drops are recommended for all breastfed babies. After the first year, parents should make sure the child is getting recommended amounts of vitamin D fortified milk. Vitamin B12 might become a problem if the parents practice a vegetarian diet that is borderline vegan, but not a common problem in ovo-lacto vegetarians since the dairy and eggs deliver sufficient amounts of vitamin B12.
Omega-3 fatty acids are essential for brain development and optimal sources of these are fatty fish. The vegetarian alternative for fish would be nuts and seeds. Since babies cannot eat nuts, also no spoonfuls of nut butter, and seeds (choking hazard) plant oils such as soy or canala oil should be added to the meals.
The plant oils also increase energy density. Low energy density can become a problem as the baby gets older. Vegetarian meals have a high nutrient and low-energy density. This is great for the parents, but not ideal for a toddler with a small stomach. Small children have a limited stomach capacity. Fiber-rich vegetarian meals might not be able to deliver the energy a child needs in the food volume a small child can eat. It is important to track the growth and fortify meals with healthy oils and lower fiber foods such as white bread or rice.
These are all hypothetical thoughts based on nutrient knowledge and experience, but is this situation also observed in real life? Only a few studies have been conducted observing babies and toddlers on vegetarian diet. These studies have found conflicting results. While some studies find no difference in height, weight, and BMI, other studies find that vegetarian children are slightly smaller than their meat-eating counterparts. There seems to be no difference in cognitive development. The only nutrient in need for close monitoring is iron after the first year of life.
Keep in mind though that we only have a few studies. Vegetarian babies and children can be healthy but parents need to be well-educated how to implement a vegetarian diet for babies and children.
Vegan Mothers and Babies
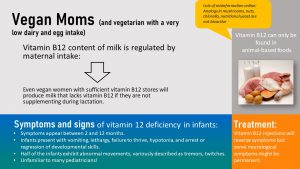
Vegans do not eat any type of animal products and this is where the most important concern comes in. Infants of vegan mothers who do not take a vitamin B12 supplement during pregnancy are born with low vitamin B12 stores. The breastmilk of vegan mothers depends on the daily vitamin B12 intake rather than liver stores. A vegan mother might not be deficient at this point because she still has sufficient stores of B12 in the liver but her breastmilk lacks vitamin B12. If the mother doesn’t supplement vitamin B12 the infant starts slipping into vitamin B12 deficiency during the first weeks of life.
Here is the problem: Vitamin B12 deficiency damages the nervous system and the symptoms are not clear and specific. Initially, the infant will be lethargic which could be interpreted as a quiet baby. Then symptoms of vomiting, hypotonia (low muscle tone), and regressing developmental skills show up. These symptoms could also indicate a viral infection. If the pediatrician asks the right questions (is the family vegan?) the infant can receive a vitamin B12 injection and soon recovers. If the deficiency is caught too late, the damage to the nervous system can be irreversible causing lifelong issues.
Aside of vitamin B12, the same nutrients that need special attention in a vegetarian diet need to be watched in a vegan’s diet as well. A vegan baby can get protein from beans and mashed or pureed tofu. Iron-fortified cereal is a great way to prevent anemia.
Vegan babies benefit from breastfeeding for more than one year, because breastmilk supplements the nutrients from plant food. If a vegan baby is weaned during the first year, they should receive iron-fortified, infant soy-based formula until 12 months. Milk alternatives (soy, rice, almond, hemp, etc.), are not recommended before 12 months because it can lead to severe vitamin, mineral, fatty acid, and amino acid deficiencies.
After 12 months, full-fat, fortified soy milk may be introduced and is a great source of calcium, vitamin B12, and vitamin D. Parents need to read the label to ensure that the soymilk is fortified.
Tooth Decay
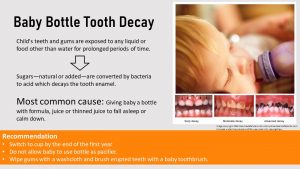
After the first six months of feeding milk, the intake of simple sugars from milk is reduced by replacing the milk progressively with vegetables, cereals, fruits, and meats. In addition, infants should be transitioned from bottle to sippy cup feeding. The reason for this recommendation are the incoming baby teeth.
Suckling on a bottle with sweet milk or juice calms the baby down, and some parents use this to put a fussy baby to sleep at night or on outings. This convenient habit is the main contributor to tooth decay in babies and toddlers which is why the condition is called baby bottle tooth decay.
Baby Bottle Tooth Decay usually occurs in the upper front teeth. While the baby is using the bottle as a pacifier the sugary liquid—this includes lactose from milk—bathes the teeth in a sugary solution for a prolonged time. Mouth bacteria feast on this sugar and produce acid which eats away on the tooth enamel. Advanced tooth decay leads to the loss of teeth.
If teeth are lost too early, the child may develop speech problems or eating problems.
Good oral hygiene is the key to prevent baby bottle tooth decay. For babies this involves wiping the gums after the bottle of milk is finished, beginning when teeth are in the process of erupting. After teeth have erupted baby’s teeth need to be brushed with a soft baby brush daily. The transition from bottle to sippy cup should be started early and be completed by 12 months.
Allergy Recommendations Have Profoundly Changed During the Last Years
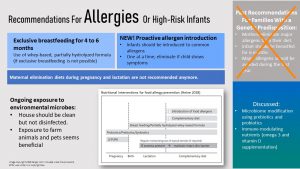
Allergies can change the baby’s diet profoundly. If allergies run in the family, parents are often willing to do everything to prevent the baby from developing an allergy because allergies have not only a major impact on family meals, but also eating at school and interactions with friends and extended family.
As explained earlier, parents should introduce solid foods one at a time to catch allergenic foods easily. If a group of foods is introduced as a meal it becomes hard to identify the culprit.
A decade ago families of infants with a high risk to develop food allergies received a long list of allergenic foods to avoid during pregnancy, breastfeeding, and once the infant started eating solids. Recently, several new studies disproved this recommendation. The old recommendations are still passed around, which makes it important that health care providers understand the shift to the new recommendations.
The new studies showed that avoiding common allergens during the first couple of years actually increases the risk for allergies. The new recommendations include:
- Infants should be exclusively breastfed for 6 months. Only if the infant develops allergies during exclusive breastfeeding, individual foods might be eliminated from the mother’s diet in consultation with the pediatrician. The elimination diets of the past (pregnancy and breastfeeding) are not recommended. If the infant develops a cow’s milk allergy a hypoallergenic formula should be fed.
- Common allergens should be introduced early on, but not before the end of the 4th month, one at a time. The studies showed that exposing infants to common allergens reduced the incidence of allergies in at risk infants.
- Exposure to a clean but not bleached home environment, to animals and a farm environment seems to activate immune system learning. By doing this, the immune system seems less likely to overreact, which basically describes an allergic reaction.
- Microbiome modification using pre- and pro-biotics are also discussed. This strategy should only be implemented by an allergist or immunologist (physician specializing in allergy or immunology) and not just “tried” by parents with an over-the-counter supplement.
Interested In More Information?
- American Academy of Pediatrics: Starting Solid Foods
- CDC: Food and Drinks for 6 to 24 Months Olds
- If you are interested in allergies, here is an article for further reading: Cleaning Up the Hygiene Hypothesis
Editors: Sydney Christensen, Eric Hanzel
NUTR251 Contributors:
- Spring 2020: Miranda Haverdink, Caleb Licking, Caroline Leibel, Danae McKenzie, Jenna Junker, Shane Rapp, Alondra Iturbide, Kennedie Engles, Eli Havekost, Haley Jensen
- Fall 2020: Megan Appelt, Morgan McCain, Peyton Hainline, Shalin Bhakta
Potential Renal Solute Load:
Amount of Na, K, P, Cl, and N (from protein and non-protein N)



Feedback/Errata